Weight Health Ecosystem: Hormones, Nutrition, and Lifestyle Intertwine
In a world increasingly defined by quick fixes and the allure of the latest medical breakthrough, this conversation with Ashley Koff, RD, challenges the very notion of "weight loss" as the ultimate goal. Instead, Koff introduces a paradigm shift towards "weight health," a holistic ecosystem where hormones, nutrition, and lifestyle intertwine. The non-obvious implication? That the current metabolic crisis, fueled by ultra-processed foods and historical dieting failures, has created a physiological environment where our natural weight regulation systems are fundamentally undermined. This conversation is essential for anyone who feels perpetually stuck in a cycle of yo-yo dieting, has experienced the limitations of traditional weight loss approaches, or is considering or currently using GLP-1 medications. It offers a strategic advantage by demystifying the complex interplay of hormones and food, providing a framework to navigate these challenges with a focus on sustainable, long-term well-being rather than just the number on the scale.
The Hidden Costs of "Enriched" Foods and the Undermining of Our Internal Systems
The conversation begins by confronting a foundational issue: the modern food supply. Ashley Koff, a former marketer of sugar-laden cereals, offers a stark perspective on how "enriched" foods, a term that sounds beneficial, are actually a marketing ploy for a product stripped of its natural nutrients. This isn't just about what's in ultra-processed foods, but critically, what's missing. Koff argues that these foods are engineered to bypass our natural satiety mechanisms, leading to a state of chronic under-fueling. This under-fueling, she explains, directly impacts our "weight health hormones"--GLP-1, GIP, PYY, and CCK--which are intricately linked to appetite, fat storage, and metabolism.
"When the ultra-processing of food happened, and we came up with marketing terms like 'enriched flour,' which is actually the opposite, it's the poorest flour, but they came up with the term enriched. I know because it was during my marketing time, and it's like, we'll make you feel rich, and enrichment sounds like it's something people want in their lives."
This systemic depletion of essential nutrients creates a feedback loop. Our bodies, not receiving the signals they need, struggle to regulate appetite and metabolism effectively. The conventional approach, often focused solely on calorie restriction or macronutrient ratios, fails to address this deeper physiological deficit. Koff emphasizes that this isn't about willpower; it's about the body's fundamental inability to function optimally due to a lack of resources. The consequence of this under-resourcing is a body that is out of balance, setting the stage for metabolic dysfunction and a reliance on external interventions like GLP-1 medications. The immediate "benefit" of these processed foods--palatability and convenience--masks a long-term cost: the degradation of our internal hormonal signaling systems.
GLP-1 Medications: A Biosimilar Tool in a Dysregulated System
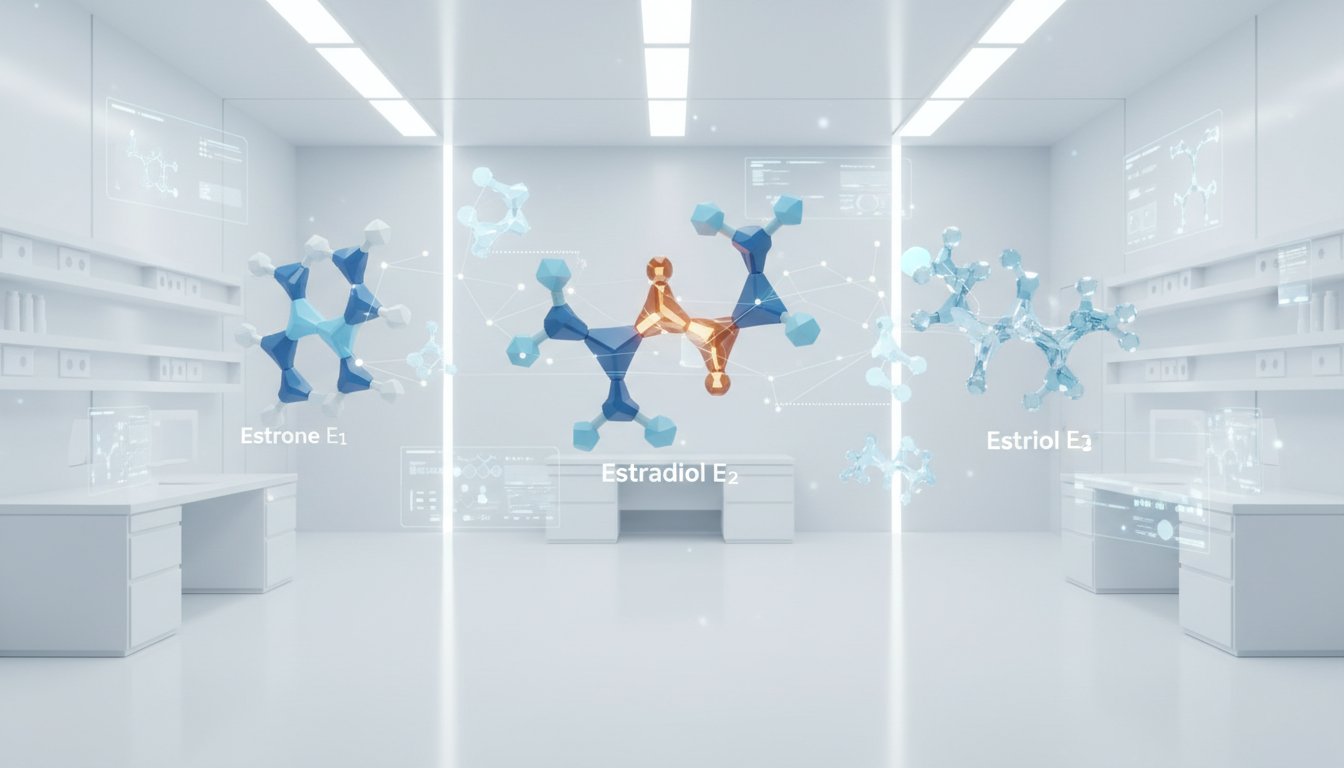
The discussion around GLP-1 medications highlights a critical distinction between bioidentical and biosimilar treatments. While hormones like insulin or thyroid medication are bioidentical, meaning they function exactly like the body's own, GLP-1 agonists are biosimilar. They work by interacting with the same receptor sites throughout the body, but they bypass the body's natural signaling and deployment processes. Koff explains that the body's natural GLP-1 signal is transient, lasting only a few minutes. Modern life, however, bombards us with constant food cues, necessitating a more sustained signal.
"The difference with these hormones, with these weight health hormone replacements, which is what semaglutide and tirzepatide are, is that they are biosimilar. So let's use that. Biosimilar means when the body receives them... it goes right to the receptor sites, which we now know thanks to these medications are all throughout our body, not just dealing with blood sugar and in the brain for satiety."
This sustained action, while beneficial for appetite control in a food-saturated environment, can lead to unintended consequences if not managed properly. Koff points out that patients can experience fatigue, digestive issues, and muscle loss when dosing and nutrition are not optimized. This is because the medication can keep the body in a constant "fight or flight" or "metabolically active" state, hindering rest and digest functions. Furthermore, delayed gastric emptying, a known effect of GLP-1s, can disrupt the gut microbiome and affect nutrient absorption. The implication here is that GLP-1 medications are powerful tools, but they are not a magic bullet. Their effectiveness and safety are heavily dependent on a holistic approach that includes optimized nutrition, appropriate dosing, and attention to the body's overall physiological state--areas often overlooked in a purely prescription-driven model. The long-term advantage of using these medications responsibly lies in their potential to restore a semblance of hormonal balance, but this requires a deeper understanding than simply taking a pill.
The Weight Health Ecosystem: Beyond Weight Loss as the Sole Objective
A pivotal insight from the conversation is the reframing of "weight loss" as "weight health." Koff argues that societal obsession with weight alone is a flawed metric that often leads to unhealthy behaviors and a failure to address underlying physiological issues. She posits that the body is a "weight health ecosystem," where every choice--sleep, food, stress--impacts hormonal balance and overall well-being. This perspective shifts the focus from a singular outcome (weight reduction) to a multifaceted process of optimizing bodily functions.
"If we realized we're a weight healthy ecosystem, then something really incredible happened. When in 2004, when I saw my first bariatric patient, I saw overnight their diabetes went away. Then I saw over the course of one week that their entire relationship with food, with appetite, with cravings, with hunger, all of that changed."
The consequence of this shift is profound: when the focus is on health, weight often follows as a byproduct. Koff shares her own journey, highlighting how traditional dieting failed her, but a focus on healing her digestion and understanding her body's hormonal signals led to sustainable change. This approach acknowledges that weight is a key performance indicator of overall health, but not the only one. Muscle mass, bone density, and metabolic markers are equally, if not more, important. The advantage of this "weight health" framework is its durability. It moves beyond temporary fixes to build a resilient body capable of maintaining health across different life stages, including the ability to potentially come off medications like GLP-1s while maintaining progress, not by stopping the medication, but by optimizing the underlying "ecosystem." This requires patience and a willingness to address discomfort now for long-term gain, a concept often at odds with the instant gratification culture.
Actionable Takeaways for Navigating Weight Health
- Prioritize Nutrient Density: Over the next quarter, focus on incorporating whole, unprocessed foods rich in essential micronutrients. Actively seek out foods that provide magnesium, B vitamins, and other vital compounds often lacking in ultra-processed options. This pays off in 6-12 months as your body's hormonal signaling improves.
- Challenge "Enriched" Labels: For the next month, be highly skeptical of products labeled "enriched." Understand that this often signifies a stripped-down product requiring artificial fortification, and opt for whole-food alternatives whenever possible. This immediate action builds awareness and shifts purchasing habits.
- Integrate Digestive Health Support: Immediately begin incorporating practices that support digestion, such as mindful eating, adequate hydration, and considering digestive enzymes or probiotics if recommended by a healthcare professional. This is crucial for optimizing nutrient absorption, which is foundational for weight health.
- Consult a Qualified Nutritionist/Dietitian Before GLP-1s: If considering GLP-1 medication, commit to working with a qualified nutrition professional before starting. This investment, ideally over 3-6 months, ensures you have a foundational understanding of nutrition and lifestyle to complement the medication, preventing potential downstream issues like muscle loss or digestive distress.
- Reframe "Weight Loss" to "Weight Health": Over the next 6-18 months, actively shift your personal and public discourse from "weight loss" to "weight health." Measure progress not just by the scale, but by improvements in energy, sleep, digestion, and strength. This mindset shift creates lasting advantage by focusing on sustainable well-being.
- Embrace Delayed Gratification: Recognize that true weight health is a marathon, not a sprint. Identify one area where you can implement a change that might feel uncomfortable now (e.g., consistent meal prep, prioritizing sleep) but will yield significant long-term benefits. This pays off in 12-24 months and beyond.
- Understand GLP-1s as Tools, Not Cures: If using GLP-1 medication, view it as a tool to support your weight health journey, not a complete solution. Commit to ongoing education about its mechanisms and potential side effects, and work with your healthcare team to optimize its use. This requires continuous engagement over the duration of use.