Menopause as Hormone Deficiency: Optimizing Health With Bioidentical Therapy
The Estrogen Family: Beyond the Single Hormone Myth and into Optimal Health
This conversation with Dr. Felice Gersh exposes the profound, often overlooked, complexity of estrogen, revealing that menopause is not merely an endpoint but a cascade of hormonal deficiencies with far-reaching systemic consequences. The hidden implication is that a simplistic view of "estrogen" leads to inadequate treatment, potentially exacerbating inflammation, autoimmune conditions, and chronic diseases. Those navigating perimenopause and menopause, or seeking a deeper understanding of women's health beyond symptom management, will gain a critical advantage by recognizing estrogen as a family of hormones with distinct roles and understanding the nuanced science behind hormone therapy. This insight empowers proactive health decisions, moving beyond fear-based approaches to embrace a more informed, personalized strategy for long-term well-being.
The Cascade of Estrone: When Inflammation Becomes the Dominant Estrogen
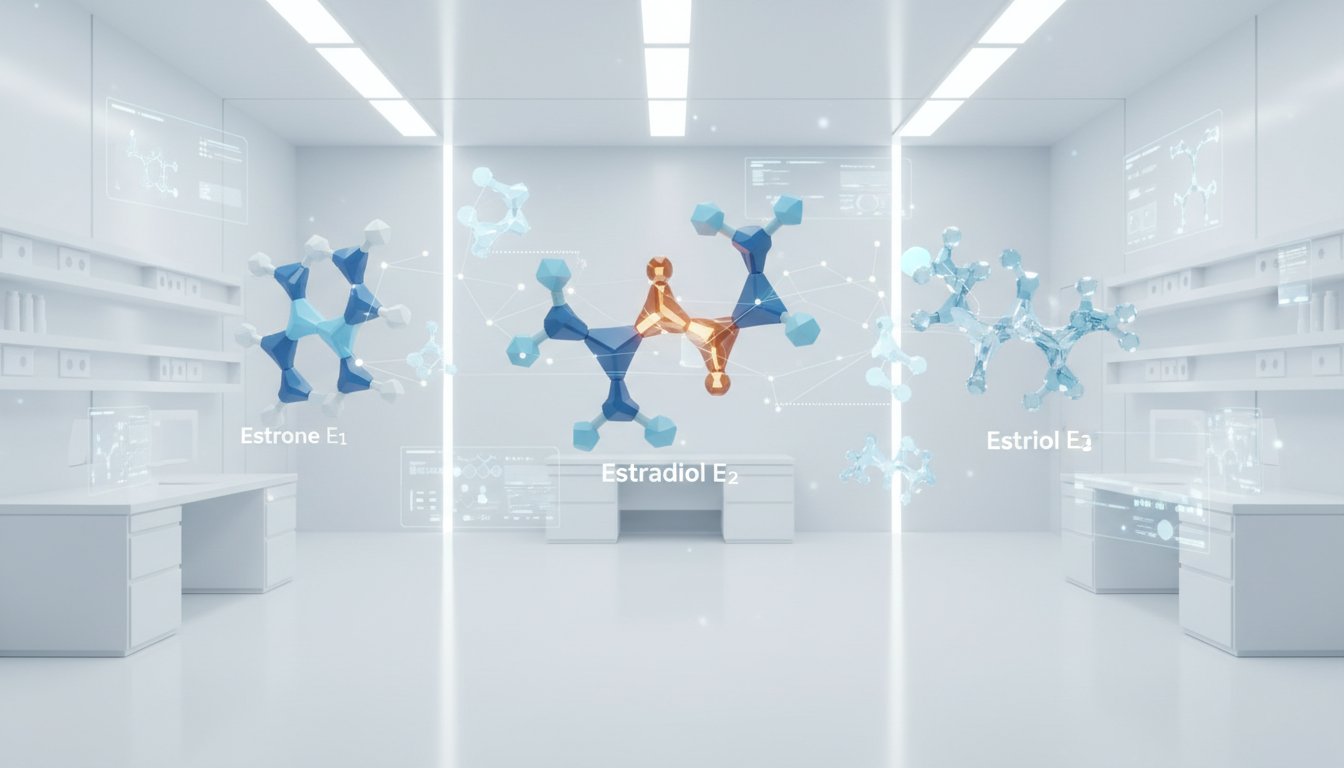
The common understanding of estrogen is a singular entity, a simplification that Dr. Felice Gersh argues is not only inaccurate but actively detrimental to women's health. In reality, estrogen is a complex family, with estradiol (E2) being the primary hormone produced by ovaries during reproductive years, estriol (E3) dominant in pregnancy, and estrone (E1) becoming prevalent post-menopause, particularly in women with excess adipose tissue or metabolic dysfunction. This shift from estradiol to estrone is not merely a change in hormone type; it signifies a fundamental alteration in the body's hormonal signaling, with profound downstream effects.
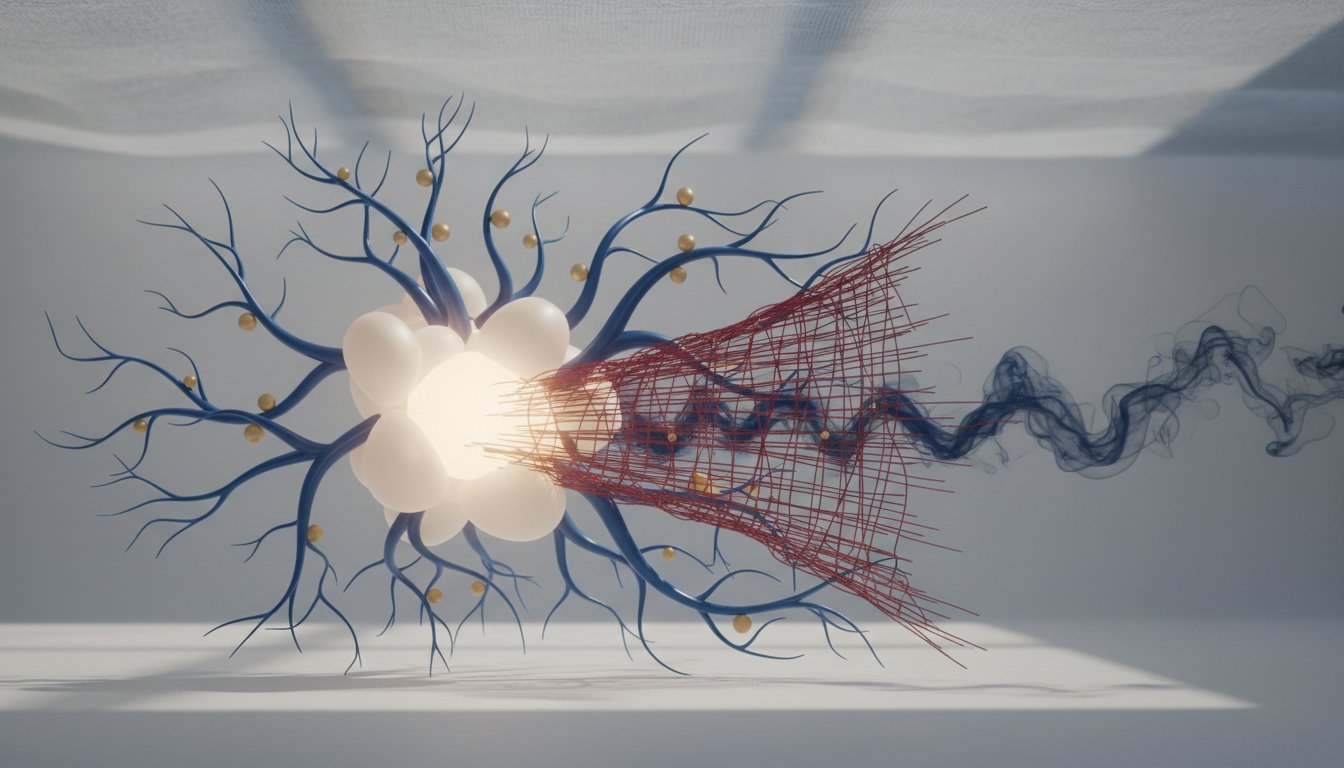
Estradiol, Dr. Gersh explains, acts as a balanced modulator across various estrogen receptors (alpha, beta, and G-protein coupled), maintaining a state of calm and anti-inflammation. Estrone, however, predominantly activates the alpha receptor. While crucial for bone and muscle health, unchecked alpha receptor activation, especially in the absence of estradiol's balancing influence, can lead to a pro-inflammatory state. This pro-inflammatory environment, exacerbated by factors like gut dysbiosis and leaky gut--conditions that worsen post-menopause due to declining estradiol--creates a vicious cycle. Inflammation activates the enzyme aromatase in fat tissue, which converts androgens into more estrone. This excess estrone, in turn, further fuels inflammation and can promote uncontrolled cell proliferation, a critical factor in the development of cancers like breast cancer. The misconception that "estrogen causes cancer" often stems from this estrone dominance, not from the beneficial effects of estradiol.
"So estrone predominantly activates alpha, and you can think of it as sort of the yin-yang kind of thing. And then there's the balance. So the alpha receptor is the dominant one on the innate immune cells. So they would be things like neutrophils, macrophages, mast cells. So they're the first responders of the immune cells of the immune system to invaders, like bacteria, viruses. That's what saves your life, you know, so you don't die of sepsis and get an infection that goes travels through your whole body or to injury, damage."
-- Dr. Felice Gersh
This understanding reframes menopause not as a natural, benign transition, but as a state of hormone deficiency that can default to a pro-inflammatory condition if not addressed. The implications are vast, extending to increased risk of autoimmune diseases, such as rheumatoid arthritis, due to molecular mimicry--where antibodies mistakenly target the body's own tissues. The body's immune system, confused by the altered hormonal landscape and the presence of toxins from a compromised gut barrier, begins to attack itself. This systemic inflammation, driven by estrone dominance, is a critical factor in many chronic health issues that emerge or worsen after menopause.
The "Low Dose for Shortest Time" Fallacy: Undermining the Potential of Hormone Therapy
The prevailing narrative around hormone replacement therapy (HRT), largely shaped by the Women's Health Initiative (WHI) study, has instilled widespread fear and caution. Dr. Gersh meticulously deconstructs this narrative, highlighting how the WHI's choice of synthetic, non-human hormones (conjugated equine estrogens from horse urine and medroxyprogesterone acetate, a synthetic progestin) and potentially suboptimal dosing regimens led to misleading conclusions. These synthetic hormones, she argues, do not mimic the molecular structure and function of human hormones and can even act as endocrine disruptors, leading to adverse effects like increased blood clotting and inflammation.
The subsequent mantra of "lowest dose for the shortest time," while intended to mitigate risk, has, in many cases, rendered hormone therapy ineffective. Studies like KEEPS and ELITE, which used lower doses or less ideal formulations, failed to demonstrate significant cardiovascular benefits, not because hormones are inherently ineffective, but because the doses used were insufficient to achieve therapeutic levels. Dr. Gersh posits that the goal of hormone therapy should not be merely symptom suppression (like hot flashes) but the restoration of physiological hormone levels to maintain optimal function across all organ systems--cardiovascular, neurological, musculoskeletal, and beyond.
"So the mantra became, if you're going to use hormones, and it was only for suppression of hot flashes and night sweats, okay? And it's still this is still the case. There's no medical organization or society that is actively promoting in their guidelines the use of hormone therapy for prevention of cardiovascular disease, for prevention of dementia, you know, and there's no neurological society."
-- Dr. Felice Gersh
This highlights a critical failure in conventional medical practice: the reluctance to embrace hormone therapy for its potential to promote long-term health and longevity, rather than just treating acute symptoms. The science supporting estradiol's role in maintaining vascular health, cognitive function, and bone density is substantial, yet it is often overshadowed by the fear generated by flawed studies using inappropriate hormone formulations. The implication is that by adhering to outdated protocols and fear-based messaging, medicine is failing to provide women with a powerful tool for optimizing their healthspan.
The Art of Hormone Replacement: Timing, Delivery, and the Promise of Bioidenticals
Dr. Gersh advocates for a more nuanced, personalized approach to hormone therapy, emphasizing the importance of timing and delivery methods. She suggests that conversations about hormone support should begin much earlier than commonly thought, ideally in the decade leading up to menopause, as ovarian aging and hormonal shifts begin long before the cessation of periods. The decline in progesterone starts in the mid-30s, and estradiol levels fluctuate significantly during perimenopause. Monitoring hormone levels, while not always mainstream, can provide valuable insights, but observable signs of aging--such as changes in skin elasticity and vaginal dryness--can also serve as potent indicators of hormonal deficiency.
The distinction between "bioidentical" (or "human-identical," as Dr. Gersh prefers) hormones and synthetic ones is crucial. Bioidentical hormones are molecularly identical to those produced by the human body, meaning they interact with receptors in the same way estradiol and progesterone do. This precise molecular match is key to their efficacy and safety profile when used appropriately. While commercial pharmaceutical-grade bioidentical hormones are available, compounding pharmacies offer flexibility in dosing and formulation, which can be essential for individuals who don't respond well to standard preparations or have unique needs.
The application of topical estradiol and estriol to the skin, for instance, is presented not just as a cosmetic intervention but as a strategic way to enhance systemic hormone levels, leveraging the skin's ability to absorb these hormones. Estriol, in particular, is highlighted for its potential benefits on skin health due to its strong affinity for beta receptors, which are prevalent in skin tissues. This approach, while perhaps unconventional to some, underscores Dr. Gersh's philosophy: to utilize hormones strategically to support optimal cellular function and healthspan, acknowledging that what is visible on the skin can be a reflection of deeper systemic processes. The key takeaway is that hormone therapy is not a one-size-fits-all solution but an art informed by science, requiring careful consideration of individual needs, appropriate hormone types, and optimal delivery methods to achieve genuine physiological balance and long-term health.
Key Action Items
- Initiate Proactive Conversations: Begin discussing perimenopausal and menopausal hormone support with your healthcare provider in your late 30s or early 40s, particularly if you have a family history of early menopause or experience early symptoms.
- Immediate Action.
- Understand Hormone Families: Educate yourself on the distinct roles of estradiol (E2), estrone (E1), and estriol (E3), and advocate for treatments that utilize human-identical estradiol.
- Immediate Action.
- Question "Lowest Dose" Mentality: Challenge the notion that the lowest possible dose of hormones is always best. Discuss achieving physiological levels with your provider to support optimal function across all organ systems.
- Immediate Action; Pays off in 6-12 months.
- Consider Topical Applications Strategically: Explore the use of topical estradiol or estriol for skin health, understanding this can also contribute to systemic hormone levels and potentially offer "more bang for your buck."
- Immediate Action; Benefits visible in 2-4 weeks.
- Prioritize Gut Health: Actively work to improve gut health through diet and lifestyle to mitigate inflammation, which is exacerbated by declining estradiol and can contribute to estrone dominance and autoimmune conditions.
- Ongoing Investment; Benefits compound over 6-12 months.
- Evaluate Tubal Ligation's Potential Impact: If considering or having undergone tubal ligation, discuss with your provider its potential impact on ovarian function and the possibility of earlier menopause.
- Longer-term consideration (1-2 years).
- Advocate for Comprehensive Hormone Therapy: Move beyond symptom management (hot flashes) and advocate for hormone therapy to support cardiovascular, neurological, and musculoskeletal health, understanding the science behind estradiol's protective effects.
- Investment for long-term payoffs (1-5 years).