Perimenopausal Hormonal Shifts Disrupt Gut Health and Amplify Symptoms
TL;DR
- Declining estradiol levels in perimenopause significantly reduce gut microbiome diversity, leading to increased intestinal permeability and new food sensitivities by compromising gut barrier integrity.
- Progesterone decline in perimenopause destabilizes mast cells, exacerbating histamine-related symptoms like migraines and abdominal pain, especially when combined with gut dysbiosis.
- Alcohol consumption in midlife is particularly detrimental as it impairs histamine detoxification pathways and increases gut intestinal permeability, contributing to a worsening of perimenopausal symptoms.
- Strength training is crucial for gut health, improving microbiome diversity and flow, while also providing a vital psychological benefit by fostering self-efficacy and resilience in women.
- The estrobolome, a gut bacteria subset metabolizing estrogen, plays a critical role in hormone balance; dysbiosis can disrupt this, impacting how women experience perimenopause and menopause.
- Carbohydrate intake, particularly from whole food sources rich in fiber, is essential for gut health and thyroid function, signaling safety to the nervous system and supporting T4 to T3 conversion.
- Birth control pills are not recommended for perimenopausal symptom management as they shut down ovarian function and reduce gut microbiome diversity, carrying significant risks without true hormonal regulation.
Deep Dive
The discussion begins by addressing the cultural conditioning of women to be hyper-capable and suppress their needs, leading to a breaking point in midlife when hormonal changes reduce resilience amidst accumulating stressors like health conditions, psychological stress, work, aging parents, and relationship issues. This period is framed not just as a challenge but as an invitation to heal and embrace one's true self.
The conversation then shifts to the gut, digestion, and the perimenopausal and menopausal transition, aiming to connect gut health with potential thyroid dysfunction and immune system issues, such as itchy eyes or a constant feeling of being unwell. Dr. Christine Maren, a medical doctor and functional medicine practitioner specializing in women's health, hormones, and gut health, is introduced as a guest who helps women navigate perimenopause by addressing root causes through personalized, holistic approaches.
Key topics covered include the differences in gut diversity between men and women, the increase in gut dysbiosis and leaky gut during perimenopause due to declining estradiol, and the resulting changes in alcohol and caffeine sensitivity and food sensitivities. A decrease in progesterone's role in potentially increasing immune function in a negative way, specifically concerning histamines, is also discussed. The importance of strength training for gut health, the complex processes of liver detoxification, and the concept of the "estrobolome"--the gut's role in metabolizing estrogen--are explored. The discussion also touches upon beneficial foods like oats and carbohydrates, the importance of fiber, and the nuanced approach to carbohydrate intake for thyroid function and immune health.
The episode highlights that perimenopausal women are often magnesium deficient, which can lead to lowered hormonal production. Magnesium is involved in over 600 biochemical reactions, influencing the production of estrogen, progesterone, and testosterone, and also disrupts thyroid function and breaks down stress hormones. Insufficient magnesium results in poor hormone production and a compromised stress response.
A significant finding is that digestive symptoms are a primary complaint of perimenopause, with studies indicating a decline in female gut microbiome diversity as women age, plateauing around age 40 and decreasing further into menopause. This reduction in diversity has downstream effects on perimenopause experience, immune function, and thyroid function, demonstrating a bidirectional relationship between hormones and gut health.
The decline of estradiol is identified as the primary influencer of this reduced gut diversity, with progesterone mainly affecting motility and thyroid hormones also playing a role. Estrogen fluctuations during early perimenopause can lead to perceived "estrogen dominance" relative to progesterone, causing symptoms like tender breasts and water retention.
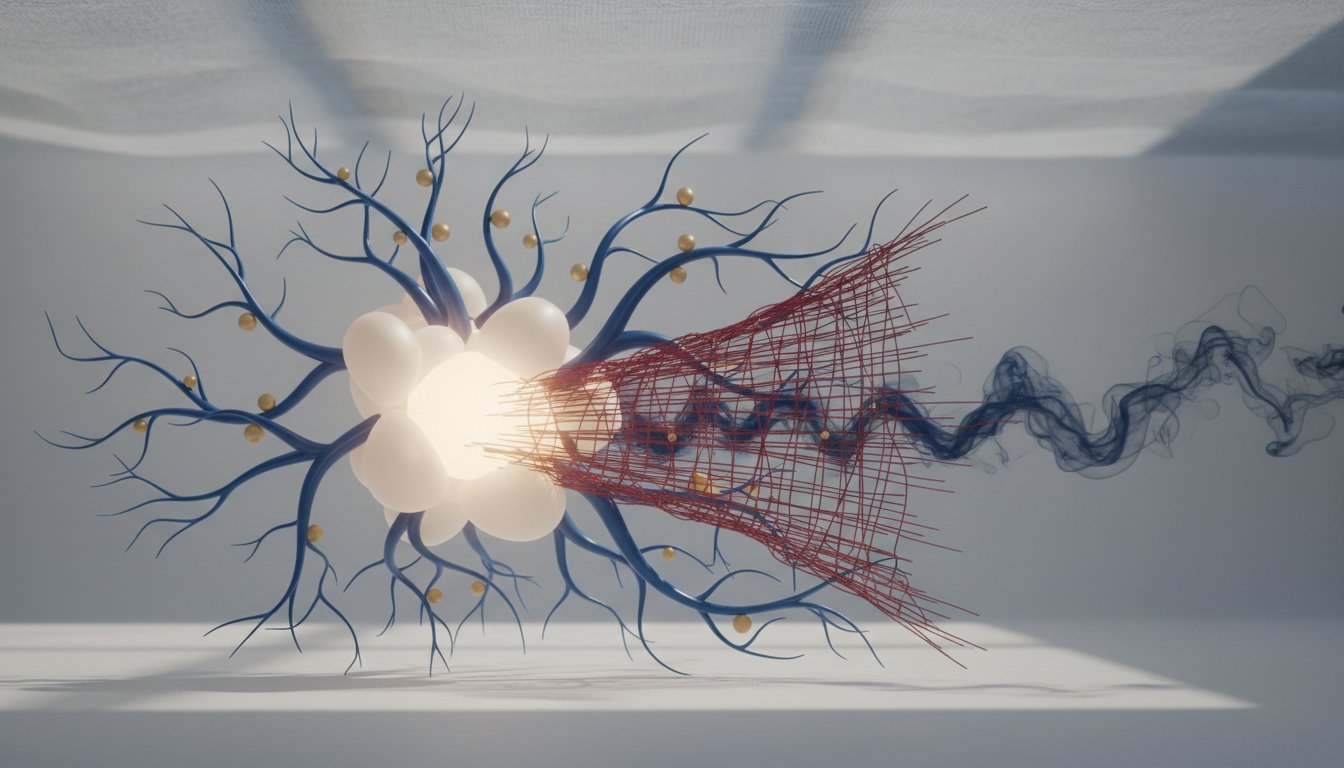
The conversation delves into how declining estradiol impacts intestinal permeability by influencing the gut's tight junctions. This increased permeability allows the immune system to react to substances it shouldn't, leading to new food sensitivities. Gut dysbiosis, characterized by a less diverse microbiome, increases the likelihood of gut infections and overgrowth of less beneficial bacteria, further contributing to intestinal permeability, inflammation, and reactions to previously tolerated foods like tomatoes, onions, garlic, bread, and alcohol. Increased rates of Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) are also documented in women going through perimenopause.
Changes in alcohol and caffeine sensitivity are discussed, with the decline in estradiol potentially affecting the ability to detoxify alcohol. While the mechanism for caffeine sensitivity is less clear, it is noted that women's capacity to metabolize substances can change. Progesterone's role in stabilizing mast cells, which release histamine, is highlighted, explaining heightened histamine issues in perimenopause, especially when combined with gut problems and estrogen dominance. Alcohol itself can be high in histamine and impair detoxification pathways, exacerbating histamine-related symptoms like runny nose, itchy skin, rashes, hives, palpitations, brain fog, headaches, migraines, and abdominal pain or hypersensitivity.
The discussion then moves to detoxification, specifically liver detoxification and its connection to estrogen metabolism. Phase I detoxification involves CYP enzymes that metabolize estrogens, while Phase II involves methylation, influenced by genes like COMT and MTHFR, and requires adequate B vitamins and magnesium. Phase III detoxification occurs through the gut, making gut health crucial for estrogen excretion. The concept of "flow" is emphasized, both in exercise and in the body's processes, including the elimination of estrogen.
The role of the "estrobolome," a subset of gut bacteria producing beta-glucuronidase, is explained. This enzyme can either promote estrogen excretion or reabsorption. While traditionally viewed negatively, it is suggested that in perimenopause and menopause, with declining estrogen levels, elevated beta-glucuronidase might be a protective mechanism for conserving estrogen. Gut dysbiosis can break this balancing switch, negatively impacting perimenopause symptoms.
The importance of hydration and electrolyte balance in perimenopause is noted, as declining estrogen affects the body's ability to retain electrolytes. Exercise, particularly strength training, is beneficial for gut health by favorably impacting the microbiome, though both excessive and insufficient exercise can lead to leaky gut. Strength training is presented as the most effective anabolic signal for muscle health, with potential benefits for muscle strength and hypertrophy that may not be consistently replicated by HRT alone.
The conversation touches upon the decline in collagen levels after menopause, affecting skin appearance and barrier function, and introduces specific skincare products designed to boost collagen. The idea that elevated beta-glucuronidase might be beneficial in an estrogen-deficient state, acting as a protective mechanism, is reiterated, emphasizing a holistic view rather than simply suppressing it with supplements like calcium d-glucarate.
A technical question is raised about whether declining estradiol impacts the specific pathways of estrogen metabolism, particularly favoring the less favorable 4-OH pathway, but the answer remains unknown. The importance of fiber and complex carbohydrates for gut health and microbial diversity is stressed, with a goal of 30 grams of fiber per day. The potential negative impact of excessive fat intake on intestinal permeability is mentioned, contrasting it with the benefits of complex carbohydrates like oats, berries, chia seeds, and flax seeds, which support gut health and can improve body composition.
The fear surrounding carbohydrates is addressed, with the speakers advocating for their inclusion, particularly for women in midlife, and challenging the demonization of foods like oats. They highlight that carbohydrates, especially those rich in fiber and color, provide essential fuel and support metabolic health. The discussion also touches upon the benefits of whole foods over processed versions, the importance of joy and flexibility in diet, and the role of strength training in supporting a healthy metabolism that can better handle carbohydrates.
The conversation pivots to the thyroid, noting that women often under-convert T4 to T3 without sufficient carbohydrate intake. Carbohydrates, along with strength training, act as safety signals to the nervous system, indicating abundance and safety, which can improve thyroid function and reduce reverse T3. Conversely, undereating and over-exercising can lead the body to conserve resources by shunting towards reverse T3, impacting thyroid function and leading to symptoms like hair loss and weight gain.
The use of ketogenic diets is discussed critically, acknowledging their potential short-term benefits for metabolic health but cautioning against long-term adherence, which can lead to an unhealthy relationship with carbohydrates and eventual weight regain. The speakers advocate for a balanced approach, emphasizing that for metabolically unhealthy individuals, a transient period of carbohydrate restriction may be beneficial, but the ultimate goal is increased
Action Items
- Audit gut microbiome diversity: Assess current diversity and identify 3-5 key bacteria groups to target for improvement (ref: female microbiome decline).
- Implement 30g daily fiber target: Track intake and increase consumption of whole fruits, oats, chia, and flax seeds to support gut health.
- Analyze alcohol and caffeine tolerance: Monitor reactions and consider reducing intake, noting potential histamine triggers and detoxification pathway changes.
- Evaluate strength training impact: Track muscle mass and strength gains, correlating with improvements in gut health and overall resilience.
- Review detoxification pathways: Identify potential bottlenecks in liver and gut phases, focusing on nutrient support for methylation and estrogen metabolism.
Key Quotes
"You know we're conditioned as children a lot of times in our culture to be hyper capable uber responsible able to take care of ourselves and suppress our own needs and we show up for everybody else all the time for a really long time and when we get to midlife and we have all these things piling up you know health conditions psychological stress work stress aging parents relationship stress all of this stuff piles up and then our hormones make us less resilient and it's just like it's like the straw that breaks the camel's back and i think it's also an invitation to heal and become more of who we are."
Dr. Maren explains that societal conditioning often leads women to prioritize others' needs over their own, a pattern that becomes unsustainable in midlife when compounded by hormonal changes and life stressors. This quote highlights how perimenopause can serve as a catalyst for women to re-evaluate their self-care practices and embrace personal healing.
"So if we look at the studies these just came out like as 10 15 years like they're pretty recent literature really when we're looking at the microbiome and we can see that the female microbiome starts to decline in diversity as we age and so the male and the female microbiome are really different that's called sexual dimorphism and the female microbiome starts to experience less diversity and plateaus around the age of 40 and so by the time we're in menopause we often have much less gut diversity and that has really big downstream effects on the way we experience menopause or perimenopause and even our immune system and thyroid function so there's this bidirectional effect between hormones and gut health for sure."
Dr. Maren points out that recent research indicates a decline in gut microbiome diversity in women as they age, particularly around the age of 40. This reduction in diversity, known as sexual dimorphism, is linked to hormonal changes during perimenopause and menopause and has significant implications for overall health, including immune function and thyroid activity. The quote emphasizes the interconnectedness of hormones and gut health.
"Estradiol influences the tight junctions in our gut and plays a direct role in intestinal permeability so as we lose that permeability and those tight junctions become more loose our immune system starts to see things on the other side that we shouldn't really see and we get more food sensitivities but it also is this aspect of dysbiosis so you know as we become or sorry gut microbiome becomes less diverse we're more likely to have gut infections you know we have less of the good bacteria keeping the balance."
Dr. Maren details how declining estradiol levels during perimenopause directly impact intestinal permeability by loosening the tight junctions in the gut lining. This increased permeability allows the immune system to encounter substances it normally wouldn't, leading to food sensitivities and dysbiosis, an imbalance in gut bacteria. The quote explains that a less diverse microbiome is less effective at maintaining a healthy gut environment.
"Progesterone stabilizes mast cells which release histamine and so loss of progesterone is going to be gonna kind of do that double whammy especially if you have underlying issues with your gut and then like you said those chaotic the hyperestrogenism you know so high estrogen compared to low progesterone is going to destabilize histamines and so when it comes to alcohol that's kind of like a double whammy when it comes to histamine right so a lot of alcohol is high in histamine but then it also impairs your histamine detoxification pathways."
Dr. Maren explains the role of progesterone in stabilizing mast cells, which are involved in histamine release, and how its decline during perimenopause can exacerbate histamine-related symptoms. She notes that this effect is compounded by gut dysbiosis and fluctuating estrogen levels, leading to a "double whammy" of histamine issues, particularly when consuming alcohol, which is high in histamine and impairs detoxification pathways.
"Estrogen is that same way we want flow we want estrogen coming in and going out we want it to happen in a healthy way and so part of that flow is then gut health making sure you're pooping every day for women who are constipated they're not going to be pooping every day but this is where the interesting stuff comes into play because your gut microbiome plays a really big role in how you break down and excrete estrogens or how you reabsorb some of them and essentially increase your levels."
Dr. Maren emphasizes the importance of "flow" for estrogen metabolism, likening it to overall bodily function. She highlights that healthy gut function, specifically daily bowel movements, is crucial for the proper breakdown and excretion of estrogen. The quote explains that the gut microbiome significantly influences whether estrogen is eliminated or reabsorbed, impacting overall hormone balance.
"I liken this to like flow everything in our body really benefits from flow when we exercise we improve flow when we have a bladder infection or uti like we want more flow flow is a really good thing so estrogen is that same way we want flow we want estrogen coming in and going out we want it to happen in a healthy way and so part of that flow is then gut health making sure you're pooping every day for women who are constipated they're not going to be pooping every day but this is where the interesting stuff comes into play because your gut microbiome plays a really big role in how you break down and excrete estrogens or how you reabsorb some of them and essentially increase your levels."
Dr. Maren uses the concept of "flow" to describe the ideal state for bodily processes, including estrogen metabolism. She connects this to exercise and the importance of daily bowel movements for eliminating estrogen. The quote explains that the gut microbiome's role in estrogen breakdown and reabsorption is critical, and constipation can disrupt this flow, potentially leading to increased estrogen levels.
"Fiber is going to help us be more regular right so we want flow bring it in bring it out if you're constipated and you're not having good healthy bowel movements we've got a problem that might influence your hormone balance it will influence inflammation and the way you hold on to toxins and all that kind of stuff so like you should poop every day if you're not let's work on that adding fiber is really critical."
Dr. Maren underscores the critical role of fiber in promoting regularity and supporting overall health. She explains that adequate fiber intake is essential for daily bowel movements, which are crucial for hormone balance, managing inflammation, and toxin elimination. The quote emphasizes that if one is not having regular bowel movements, increasing fiber intake is a key intervention.
"The estrobolome is the subset of gut bacteria that make beta glucuronidase and beta glucuronidase is the enzyme to turn off or turn on the switch that tells us to get rid of estrogen or let's conserve and bring it back in and when we experience perimenopause or menopause let's just go to menopause when we experience perimenopause and our gut microbiome is really healthy our body might say hey you know what we've got low estrogen levels let's reabsorb some of that to protect you on the flip side when we experience let's say i don't know some high estrogen state maybe
Resources
External Resources
Books
- "Female Centric Ketogenic Diet" by Dr. Stephanie - Mentioned as a book written by the podcast host, discussing a ketogenic diet paired with the menstrual cycle for individuals who are metabolically unhealthy.
Articles & Papers
- "Studies on high fat diets and how they impact intestinal permeability" - Discussed as research indicating that higher fat diets, particularly those with saturated fats, can cause a transient increase in intestinal permeability.
- "Meta-analyses on HRT and strength gains" - Mentioned as research with mixed results regarding the benefit of hormone replacement therapy (HRT) on strength gains, leading to the conclusion that strength training is paramount.
- "Pubmed articles on oats" - Referenced as a source for those interested in reading scientific articles about the benefits of oats.
People
- Dr. Christine Maren - Guest, medical doctor and functional medicine certified practitioner specializing in women's health, hormones, and gut health.
- Dr. Stephanie Astima - Host of the podcast "BETTER! Muscle, Mobility, Metabolism & (Peri)Menopause," author, and practitioner.
- Harley Pasternak - Mentioned as a guest on the show who has a daily cookie ritual.
- Jenny - President of Strong Fitness, who introduced Dr. Stephanie to Dr. Christine Maren.
Organizations & Institutions
- Strong Fitness - Magazine mentioned as having featured both Dr. Stephanie and Dr. Christine Maren on its cover.
Websites & Online Resources
- bioptimizers.com/better - URL provided for an exclusive offer on a magnesium supplement, with promo code "better."
- peaklife.com/drstima - URL provided for a hydration protocol with a discount offer.
- oneskin.co/better - URL provided for a skincare product line with a discount code.
- manukora.com/better - URL provided for a sale on Manuka honey products.
- drinkag1.com/stephanie - URL provided for a purchase of AG1 with a free frother.
Other Resources
- Estrobolome - Defined as the subset of gut bacteria that make beta-glucuronidase, influencing estrogen metabolism.
- MTHFR - Mentioned as a genetic factor that might become more relevant in certain life stages.
- COMT - Referenced in relation to methylation and estrogen detoxification.
- Sex Hormone Binding Globulin (SHBG) - Mentioned as a marker that can increase to protect the body.
- Beta-glucuronidase - Discussed as an enzyme involved in estrogen detoxification and reabsorption.
- Small Intestinal Bacterial Overgrowth (SIBO) - Identified as a common gut infection.
- Fungal Overgrowth (SIFO) - Identified as a type of gut overgrowth.
- H. pylori - Mentioned as a potential gut infection.
- Hormone Replacement Therapy (HRT) - Discussed as a potential treatment option for perimenopausal symptoms.
- Combined Oral Contraceptives (Birth Control Pill) - Discussed as a treatment option for irregular cycles in perimenopause, with associated risks and benefits analyzed.
- GLP-1 microdosing - Mentioned as a potential therapeutic option for individuals with metabolic issues.
- Calcium D-Glucarate - Mentioned as a supplement sometimes used to address high beta-glucuronidase.
- Digestive Enzymes - Discussed as a potential replacement therapy for digestive support.
- Hydrochloric Acid (HCl) - Mentioned as a digestive enzyme that some women may need.
- Ox Bile - Mentioned as a supplement to support gallbladder function.
- Bitters - Mentioned as a support for gallbladder function.
- Pancreatic Elastase - Discussed in the context of pancreatic enzyme insufficiency.
- Low-Carbohydrate Diet - Mentioned as a potential transient elimination diet.
- Gluten-Free Diet - Mentioned as a dietary approach for individuals with digestive issues or autoimmune disease.
- Paleo Diet - Mentioned as a dietary approach.
- Mediterranean Diet - Mentioned as a dietary approach.
- Omnivore Diet - Mentioned as a dietary approach.
- Ketogenic Diet - Discussed as a dietary approach, particularly for metabolically unhealthy individuals.
- Fiber - Emphasized as critical for microbial diversity and gut health.
- Protein - Prioritized for building muscle.
- Complex Carbohydrates - Discussed as beneficial for gut health, blood sugar, and thyroid function.
- Resistant Starch - Highlighted as a beneficial type of fiber.
- Polyphenols - Mentioned as beneficial compounds found in berries.
- Micronized Progesterone - Mentioned as a potential supplement for sleep support.
- HRT (Hormone Replacement Therapy) - Discussed in relation to its potential benefits for resilience and sleep.
- Vaginal Estrogen - Mentioned as a treatment option.
- Progesterone - Discussed in relation to its role in stabilizing mast cells and histamine response.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.
- Progesterone - Discussed in relation to its role in stabilizing mast cells.
- Estradiol - Discussed as a key hormone influencing gut diversity.
- Testosterone - Mentioned as playing a role in gut health.
- Thyroid Hormones - Discussed in relation to their impact on the gut.
- T3 - Mentioned in relation to thyroid hormone conversion.
- Reverse T3 - Mentioned in relation to thyroid hormone conversion.