Facelift Recovery: Proactive Healing, Mindset, and Advanced Protocols
This episode of Well Beyond 40 delves into the complex realities of undergoing a facelift, moving beyond the superficial desire for youth to explore the intricate decision-making, unexpected complications, and powerful recovery strategies that define the experience. The core thesis is that while the immediate outcome of cosmetic surgery is often the focus, the true value lies in the meticulous preparation, the resilience in the face of adversity, and the strategic application of recovery tools. This conversation reveals hidden consequences such as the potential for severe hematomas arising from seemingly minor post-operative actions and the prolonged impact of seemingly manageable complications. Anyone considering cosmetic surgery, or indeed any significant medical procedure, will find immense advantage in understanding the full spectrum of potential outcomes, the critical importance of surgeon selection, and the systemic approach to healing that can mitigate risks and accelerate recovery. It’s a masterclass in managing expectations and leveraging resources when things don't go according to plan.
The Cascading Consequences of Cosmetic Surgery Decisions
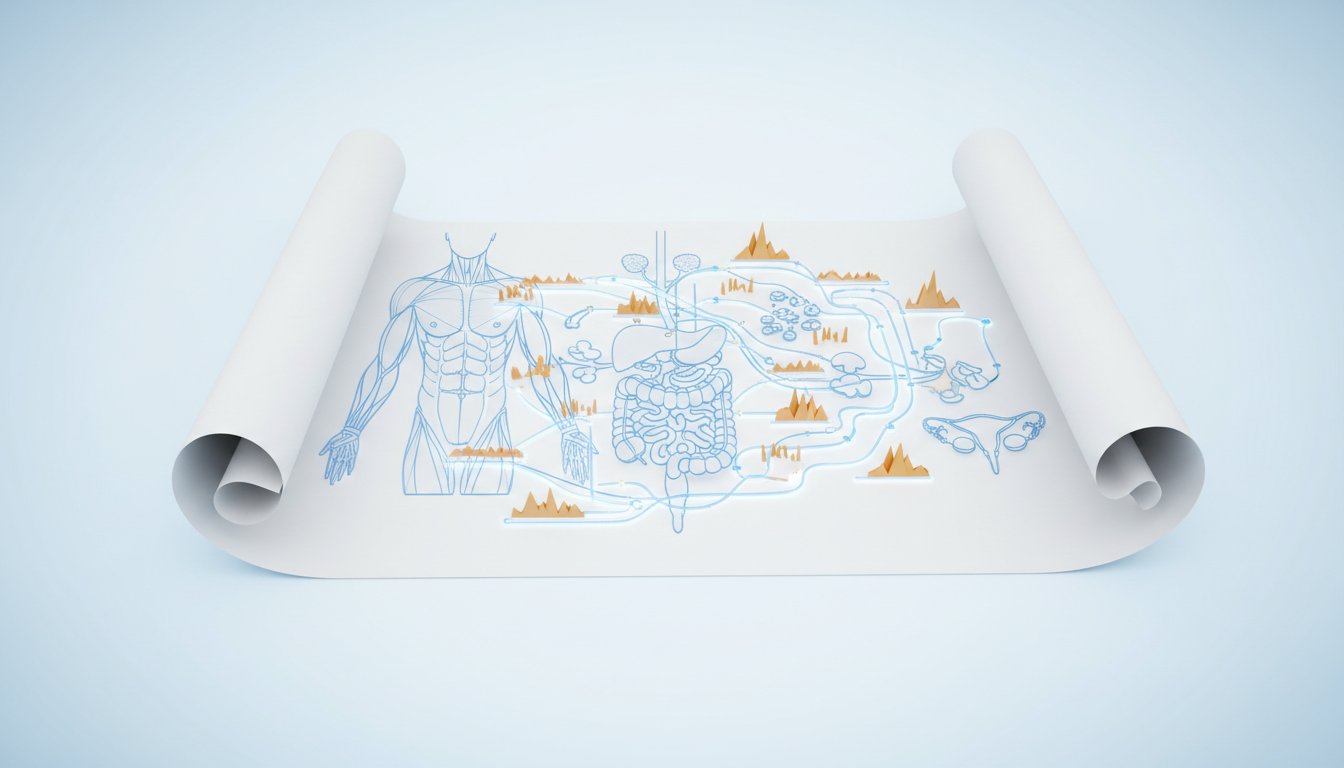
The decision to undergo a facelift, as JJ Virgin shares, is rarely a simple one. It's often the culmination of years of addressing perceived imperfections through less invasive means, a journey that, in retrospect, highlights a critical system dynamic: the escalating escalation of interventions. What begins with topical treatments or occasional Botox can, over time, necessitate more frequent and intense procedures, creating a cycle of diminishing returns and increasing cost. This isn't a failure of the initial treatments, but rather a natural progression where the body's response and the evolving aesthetic goals demand more. The implication here is that what seems like a prudent, gradual approach to aging can, in fact, lead down a path of increasingly complex and time-consuming interventions.
Virgin’s narrative illustrates how the perceived "need" for more frequent treatments--Botox, fillers, lasers--becomes a driver for considering more significant surgery. The conventional wisdom often suggests delaying such procedures as long as possible, fearing a "pulled" or unnatural look. However, Virgin encountered a counter-narrative, influenced by observing others and reading articles, suggesting that earlier intervention can yield better outcomes. This challenges the common understanding, implying that waiting too long might actually be detrimental, leading to a system where the face and body become increasingly misaligned, causing frustration and self-consciousness. The hidden consequence of this delayed approach is not just aesthetic, but emotional, impacting one's self-perception and how they "show up in the world."
"I had thought it was the opposite. I thought that you wanted to put this off as long as possible, that this wasn't something you did more than once, that it could make you look older. I had all this narrative going on that turns out are actually not true."
This realization is pivotal. It suggests a systemic flaw in how many people approach cosmetic procedures -- a focus on the immediate, visible problem rather than the long-term cascade of interventions and their cumulative effects. The advantage for those who grasp this is the potential to make more strategic decisions, potentially opting for a more significant procedure earlier, which might ultimately be more time-efficient and cost-effective than a prolonged series of less impactful treatments.
The Hematoma: When a Simple Action Triggers a Systemic Crisis
The most dramatic illustration of consequence mapping in this narrative is the post-operative hematoma. Virgin meticulously details her preparation, including a robust regimen of peptides, topicals, and advanced healing technologies like hyperbaric oxygen therapy (HBOT) and red light therapy. She also notes her pre-existing spinal injury, which made prolonged positioning uncomfortable, and her decision to take Valium for relaxation during the procedure. These elements, seemingly minor or even beneficial, converge to create a precarious situation. The critical misstep, however, was taking Oxycodone, a painkiller she knew from experience could induce nausea.
The immediate cause of the hematoma was vomiting after surgery. This act, seemingly a simple physiological response, triggered a cascade of severe complications. The pressure from vomiting caused bleeding within the surgical site, leading to a massive hematoma that swelled her face and turned it black and blue. This wasn't a minor setback; it required immediate surgical intervention to drain the hematoma and, on the following day, a further procedure to reopen the site and address its recurrence. The consequence of this single action--taking a medication known to cause nausea--was a significant delay in recovery, intense physical distress, and the potential for permanent aesthetic damage, all of which threatened her ability to meet a critical professional commitment: speaking on a stage in ten days.
"So I threw up, and when I did, it caused a hematoma. And that's like the big no-no. And you will see a picture, oh my gosh, like I went from, 'You look fine,' to 'What the heck?' like scary monster in an hour."
This situation starkly demonstrates how a seemingly isolated decision can have far-reaching, systemic consequences. It underscores the importance of understanding not just the intended benefits of medical interventions but also their potential adverse interactions and the critical role of patient adherence to post-operative instructions. The conventional approach might focus on the surgeon's skill and the initial procedure, but the hematoma incident reveals that the patient's actions, even those seemingly unrelated to the surgery itself, can dramatically alter the outcome. The delayed payoff here isn't aesthetic; it's the hard-won knowledge that meticulous attention to post-operative care, even when feeling unwell, is paramount.
Strategic Healing: Turning Immediate Pain into Lasting Advantage
Faced with a severe hematoma and a looming professional deadline, Virgin's recovery transformed into an intensive, strategic campaign. This is where the narrative shifts from managing complications to actively engineering a rapid and effective healing process, creating a distinct advantage. Her response was not passive; it was a deliberate, multi-pronged approach that leveraged her existing knowledge and resources.
She doubled down on her pre-operative regimen, increasing the frequency and intensity of treatments. This included using her home hyperbaric chamber for 90 minutes daily, applying red light therapy twice a day with a specialized mask, and continuing with the prescribed peptides (BPC-157, TB-500) and topicals. Crucially, she also incorporated IPL (Intense Pulsed Light) treatments, a procedure she had found effective for skin issues in the past. The immediate pain and alarming appearance of the hematoma were met with a systematic application of healing modalities.
The success of this aggressive recovery strategy is evident in her ability to present on stage just ten days after a significant surgical complication. This rapid turnaround, which would be astonishing under normal circumstances, becomes a testament to the power of proactive, layered healing. The advantage gained is not just about meeting a deadline; it's about demonstrating a profound capacity to manage and overcome adverse events through informed action. This approach highlights that while complications are undesirable, the response to them can create a powerful competitive advantage, showcasing resilience and mastery over the healing process.
"So I literally do it five times before I'm going off to Vegas. And by time, like I do it on a Friday, then I do it on a Monday, Wednesday, Friday, and I'm now looking at over the weekend, I'm leaving the following Wednesday, and I'm like, 'Okay, this is actually going to work out.'"
This experience suggests that conventional recovery timelines are often based on standard care, not optimized healing. By investing heavily in advanced recovery tools and treatments, Virgin effectively compressed her healing period. The lesson here is that immediate discomfort and investment in recovery protocols can lead to significant long-term payoffs, not just in terms of returning to normal life quickly, but in building confidence and demonstrating a robust approach to health management. The conventional wisdom might be to rest and wait; the advanced strategy is to actively participate in and accelerate the healing process, turning a potential disaster into a demonstration of resilience and effective intervention.
Key Action Items
-
Immediate Action (Within 1 week):
- Consultation with Multiple Surgeons: Seek out surgeons with extensive experience in the specific procedure you are considering. Prioritize those who emphasize clear communication about risks and recovery.
- Comprehensive Pre-Operative Health Assessment: Get baseline lab work done, specifically focusing on inflammatory markers and nutrient levels (e.g., Omega-3 index). Understand your body's readiness for surgery.
- Medication Review: Critically evaluate all medications and supplements, identifying any that could increase bleeding risk or cause adverse post-operative reactions (e.g., nausea-inducing drugs).
-
Short-Term Investment (1-3 Months):
- Optimize Anti-Inflammatory Diet: Ensure your diet is rich in anti-inflammatory foods and balanced in Omega-3 and Omega-6 fatty acids. This may require dietary changes or targeted supplementation.
- Source Key Recovery Tools: Invest in or arrange access to hyperbaric oxygen therapy and red light therapy devices/clinics. These are critical for accelerating tissue repair.
- Peptide Consultation (Optional, with medical guidance): Discuss the potential use of peptides like BPC-157 and TB-500 with a qualified healthcare provider to support healing.
-
Mid-Term Investment (3-6 Months):
- Establish a Consistent Healing Protocol: Develop a routine for using recovery tools (HBOT, red light) that can be implemented immediately post-procedure.
- Build a Support System: Identify trusted individuals or professionals who can provide support during the recovery period, especially if complications arise.
-
Long-Term Investment (6-18 Months):
- Mindset Cultivation: Practice mental resilience techniques to manage anxiety and maintain a positive outlook, especially if unexpected challenges occur during recovery. This "mental toughness" can be a significant factor in overcoming setbacks.
- Continuous Health Monitoring: Regularly assess key health markers to ensure your body remains in an optimal state for healing and long-term well-being, understanding that recovery is an ongoing process.