Stress-Induced Gut Distress: Low FODMAP as a Temporary Reset
This conversation with JJ Virgin, host of the Well Beyond 40 podcast, reveals a critical, often overlooked, connection between intense psychological stress and severe digestive distress. While many focus on diet as the sole driver of gut health issues, Virgin's personal experience highlights how even a "perfect" diet can become problematic when the body's stress response is chronically activated. This piece is for anyone experiencing unexplained bloating, pain, or food sensitivities, offering a systems-level understanding of how stress disrupts the gut microbiome and barrier function, and how a temporary, targeted approach like the low FODMAP diet can serve as a crucial reset. Understanding these non-obvious implications can empower readers to address the root causes of their discomfort, moving beyond symptom management to genuine healing and long-term resilience.
The Stress-Induced Gut Cascade: When Healthy Foods Turn Hostile
The immediate reaction to digestive distress often involves scrutinizing one's diet. We meticulously track macronutrients, cut out gluten, dairy, or sugar, and still, the bloating, pain, and inflammation persist. JJ Virgin's experience, however, unearths a potent, often underestimated culprit: chronic stress. Her narrative powerfully illustrates how a period of intense stress completely rewired her gut, transforming foods she'd consumed for years without issue into triggers for significant discomfort. This wasn't a simple dietary misstep; it was a systemic breakdown where stress acted as the primary catalyst.
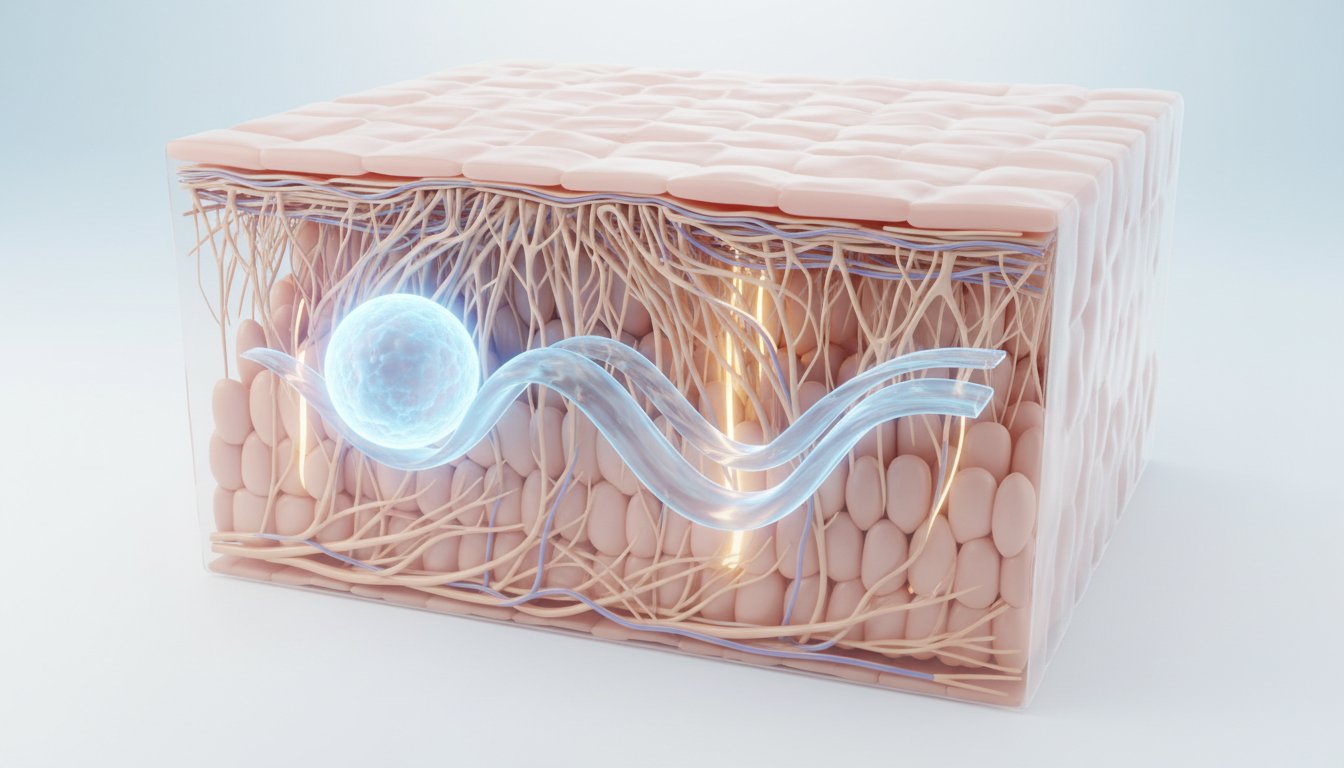
Virgin describes how stress disrupted her microbiome, leading to a decrease in beneficial bacteria and an overgrowth of opportunistic ones. This imbalance created an environment akin to small intestinal bacterial overgrowth (SIBO), resulting in constant bloating. Concurrently, her stomach acid levels dropped, impairing protein digestion and allowing more bacteria to survive and travel further down the digestive tract. Perhaps most critically, stress increased gut permeability--the dreaded "leaky gut." This condition allows undigested food particles and inflammatory compounds to cross the gut lining, directly activating the immune system below.
"Stress isn't just a feeling; it actually changes your biology."
This cascade explains why previously tolerated foods suddenly cause reactions. The compromised gut barrier and activated immune system create a heightened state of sensitivity. Virgin’s personal journey underscores that while dietary interventions like her Virgin Diet are foundational for identifying food intolerances, they may not be sufficient when the underlying stress response is wreaking havoc. This is where the low FODMAP diet emerges not as a permanent lifestyle, but as a strategic, short-term therapeutic tool.
The Low FODMAP Diet: A Temporary Respite, Not a Permanent Prison
The acronym FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are specific types of carbohydrates that are poorly absorbed in the small intestine. When they reach the large intestine, gut bacteria ferment them, producing gas and drawing water into the gut. For a healthy gut, this process is manageable. However, in a compromised gut--whether due to stress, SIBO, or inflammation--this fermentation can lead to significant symptoms like bloating, pain, gas, diarrhea, or constipation.
Crucially, Virgin emphasizes that FODMAPs are not inherently "bad." Many are found in nutrient-dense, healthy foods. The problem arises when the gut’s capacity to handle them is diminished.
"FODMAPs are not the enemy. They're simply fermentable carbs that can cause symptoms in a compromised gut."
Her experience with the diet was transformative. Within days, the "nine months pregnant" look subsided, replaced by a noticeable reduction in cramping and bloating. This immediate relief highlights the diet’s effectiveness as a short-term reset. However, the significant challenge lies in the restrictive nature of the diet. Foods like onions, garlic, broccoli, cauliflower, apples, and mushrooms--many of which are staples in a health-conscious diet--are high in FODMAPs. Virgin notes that her go-to vegetables were largely off-limits, leading to a temporary reliance on lean proteins, limited low-FODMAP vegetables (like parsnips, turnips, zucchini, and carrots), berries, gluten-free grains, and healthy fats like avocado and olives.
The danger, as Virgin points out, is viewing this as a permanent solution. Prolonged restriction can lead to nutrient deficiencies, further disrupt the microbiome by eliminating fermentable fibers necessary for beneficial bacteria, and foster an unhealthy relationship with food. The true power of the low FODMAP diet, therefore, lies in its temporary nature and its role as a stepping stone to reintroduction and long-term gut healing.
Rebuilding Resilience: From Restriction to Diversification
The ultimate goal, as articulated by Virgin, is not to live on a limited diet indefinitely, but to heal the gut sufficiently to reintroduce a wide variety of nourishing foods. This transition requires a multi-faceted approach that addresses both the immediate symptoms and the root causes.
The first step after finding relief on a low FODMAP diet is to begin reintroducing foods systematically. This process, mirroring the principles of The Virgin Diet, involves careful observation and food logging to identify specific sensitivities. Virgin’s own reintroduction has been cautious; she avoids overloading her system with high-FODMAP foods as she once did, instead adding them back in small amounts and monitoring her body's response. This mindful approach prevents a relapse into symptomatic distress.
Simultaneously, the focus must shift to actively healing and rebuilding the gut lining and microbiome. This involves incorporating gut-supportive nutrients and practices:
- Collagen and Bone Broth: These provide amino acids essential for repairing the gut lining.
- Fiber: Crucial for feeding beneficial gut bacteria, fiber intake needs to be managed carefully during reintroduction, starting low and gradually increasing.
- Fermented Foods: While potentially triggering initially, fermented foods like yogurt, kefir, and sauerkraut are vital for repopulating the gut with diverse beneficial microbes.
- Digestive Enzymes and Stomach Acid Support: These aid in breaking down food, reducing the burden on the gut.
- Sleep: Adequate, quality sleep is fundamental for bodily repair and stress management.
However, the most profound insight from Virgin's experience is the critical need to address the initial stressor. Her own gut issues were directly linked to the overwhelming pressure of a book deadline. The solution wasn't just dietary; it was a significant lifestyle adjustment--pushing back the deadline and consciously reducing her commitments. This highlights a core principle of systems thinking: interventions must address the entire system, not just isolated symptoms. If stress is the root cause, managing stress resilience becomes as vital as managing food intake.
"The bottom line is, and here's the takeaway: stress can break down your gut, but you can also rebuild it."
This requires proactive strategies for stress resilience, whether through meditation, breathwork, or simply spending more time with loved ones. The low FODMAP diet, in this context, is a powerful, temporary ally--a tool to calm the storm within the gut, creating the necessary space and stability for deeper healing and the eventual return to a diverse, enjoyable way of eating. It’s about understanding the interconnectedness of stress, biology, and digestion, and leveraging that knowledge for lasting well-being.
Key Action Items
-
Immediate Action (0-2 Weeks):
- Self-Assessment: Honestly evaluate recent or ongoing high-stress periods. Are you experiencing new or worsening digestive issues?
- Dietary Audit: Review your current diet. Are you consuming many high-FODMAP foods like onions, garlic, certain fruits, or cruciferous vegetables regularly?
- Begin Food & Symptom Logging: Use an app like Cronometer or a simple notebook to track what you eat and any digestive symptoms. This is vital for identifying patterns.
- Prioritize Sleep Hygiene: Aim for 7-9 hours of quality sleep per night.
-
Short-Term Investment (2-8 Weeks):
- Consider a Low FODMAP Reset: If symptoms are severe and persistent, consult a healthcare professional or registered dietitian to guide you through a temporary low FODMAP elimination phase.
- Incorporate Gut-Healing Nutrients: Begin supplementing with collagen peptides or bone broth protein daily. Consider adding a broad-spectrum digestive enzyme with meals.
- Implement Stress Reduction Techniques: Dedicate 10-15 minutes daily to practices like deep breathing, meditation, or gentle yoga.
-
Medium-Term Investment (2-6 Months):
- Systematic FODMAP Reintroduction: Work with a professional to carefully reintroduce FODMAP groups one by one, noting tolerance levels. The goal is to expand your diet, not restrict it further.
- Focus on Microbiome Diversity: Gradually increase intake of low-FODMAP fermented foods (e.g., lactose-free yogurt, small amounts of sauerkraut brine) and diverse low-FODMAP fruits and vegetables.
- Address Lifestyle Stressors: Make conscious changes to reduce ongoing stressors. This might involve delegating tasks, setting boundaries, or adjusting work commitments. This is where long-term advantage is built.
-
Longer-Term Investment (6-18 Months):
- Maintain a Diverse, Nourishing Diet: Aim for a wide variety of foods, incorporating previously restricted FODMAPs as tolerated, to support a robust microbiome.
- Sustained Stress Resilience: Continue practicing stress management techniques as a non-negotiable part of your health routine. This pays off in sustained gut health and overall well-being, creating a significant competitive advantage against future stressors.
- Regular Gut Health Support: Continue with foundational gut support like collagen and consider probiotics strategically based on individual needs and tolerance.