Sperm Quality Predicts Men's Longevity and Whole-Body Health
The Silent Crisis in Men's Health: Sperm Quality as a Vital Sign for Longevity and Well-being
The alarming decline in male fertility and reproductive health is not merely a concern for family planning; it's a profound indicator of broader systemic issues affecting men's overall health and longevity. This conversation with Dr. Michael Eisenberg reveals that sperm quality serves as a critical, often overlooked, vital sign, predicting not just reproductive capacity but also long-term health outcomes, including mortality risk. The implications are stark: conventional approaches to men's health and fertility are insufficient, failing to grasp the interconnectedness of metabolic health, environmental exposures, and hormonal balance. Those who understand these hidden consequences gain a significant advantage in proactively managing their health and vitality, moving beyond mere symptom management to address the root causes of declining well-being. This analysis is crucial for any man seeking to understand his health beyond the surface, and for partners and healthcare providers who wish to offer more comprehensive care.
The Unseen Predictor: Why Sperm Quality Matters Far Beyond Fertility
The narrative around infertility has historically placed the burden on women, with men often overlooked in the diagnostic process. Dr. Michael Eisenberg highlights a critical oversight: approximately half of all couples experiencing infertility have a male factor, yet men are frequently not evaluated. This lack of awareness extends to the profound implications of semen quality, which Dr. Eisenberg posits as a "sixth vital sign." The data is striking: a man's semen quality at age 40 can predict his mortality risk decades later, a correlation that appears stronger than that of smoking or diabetes. This suggests that the factors degrading sperm health are deeply intertwined with those that compromise overall systemic health and longevity.
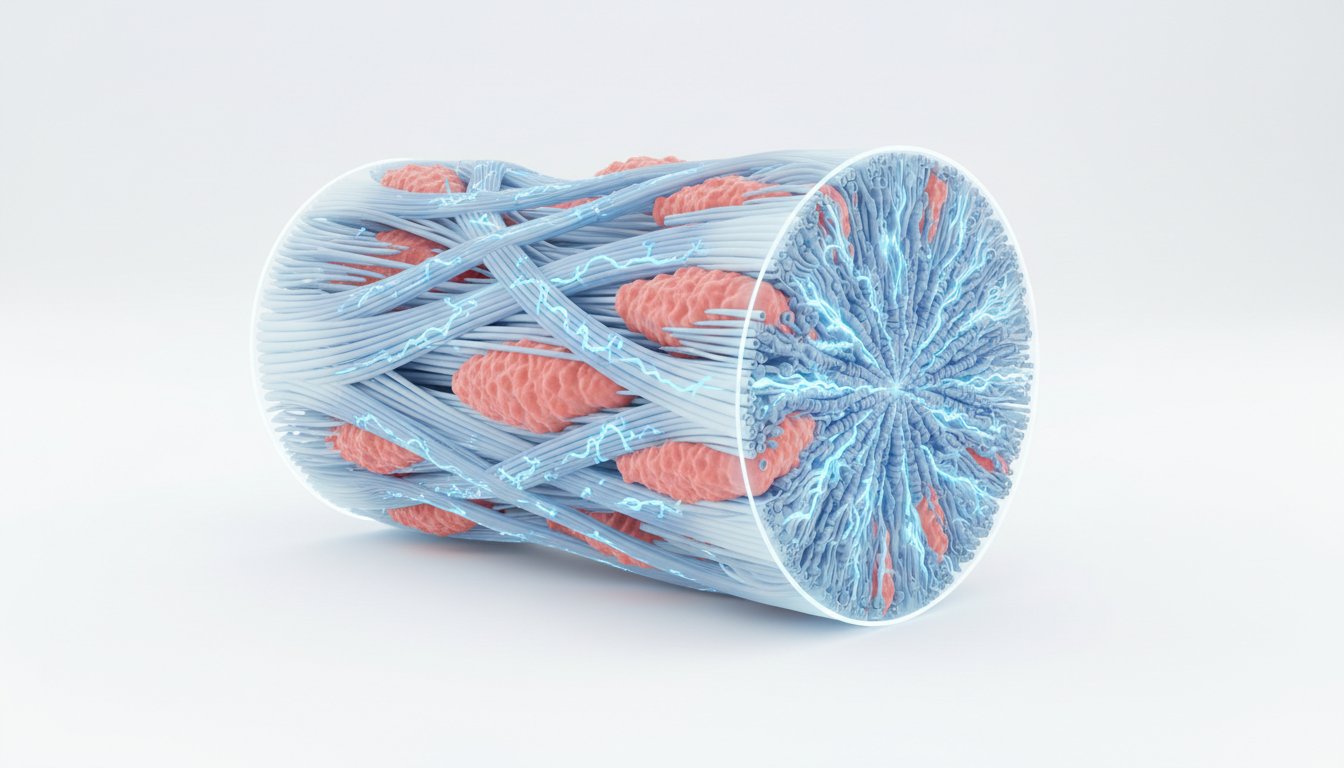
The decline in semen quality--count, motility, and morphology--has been accelerating over the past two decades, pointing to environmental or lifestyle factors rather than genetics. Dr. Eisenberg notes the ubiquity of microplastics in testicles and semen, alongside hypothesized contributions from endocrine-disrupting chemicals found in plastics and pesticides. These disruptors can interfere with hormonal signaling, potentially lowering testosterone and impacting sperm production.
"When we look at fertility through the lens of whole-body health, it changes how we think about prevention, risk, and longevity. Male fertility isn’t just about reproduction. It’s a signal."
This signal is further amplified by metabolic health. A larger belly, Dr. Eisenberg states, directly correlates with worse sperm quality and function. This connects to the broader issue of rising rates of obesity and metabolic dysfunction, which drive down testosterone levels--a trend observed even in younger men. The interconnectedness is clear: poor metabolic health, characterized by insulin resistance and excess abdominal fat, not only impairs testosterone production but also negatively affects sperm viability.
The implications of declining sperm quality extend beyond the individual man. Paternal age is increasingly linked to adverse outcomes in offspring, including neurodevelopmental disorders like autism and schizophrenia, as well as increased risks of miscarriage and preterm birth. This is attributed not only to accumulated DNA mutations over time but also to epigenetic changes--modifications to gene expression that can be influenced by a father's health and environmental exposures. These epigenetic markers, passed down through sperm, can alter fetal development and long-term health trajectories, underscoring the profound, generational impact of paternal health.
Beyond the Obvious: Lifestyle’s Cascading Effects on Reproductive Health
The conventional wisdom often fails to connect immediate lifestyle choices to downstream reproductive and overall health consequences. Dr. Eisenberg emphasizes that while many factors contribute to declining sperm quality, actionable steps can be taken. He points to the detrimental effects of scrotal heat exposure from hot tubs, saunas, and laptops, which can impair sperm production for months, as sperm regeneration takes approximately 74 days. Similarly, sedentary lifestyles and prolonged cycling, especially with certain saddle designs, can negatively impact both sperm quality and erectile function due to heat and potential nerve compression.
"It’s interesting, there is a large study done in Denmark where they had semen quality of about 50,000 men. And when that was done, they were then able to... Interestingly, where their semen quality was when they were 40 predicted their death 30, 40 years later. Wow."
The impact of alcohol is dose-dependent, with significant declines in sperm motility observed at around 20 drinks per week. Even stress, through elevated cortisol, can counteract testosterone production and negatively affect testicular function. These are not isolated incidents but part of a complex system where daily habits create cascading effects on hormonal balance and reproductive capacity.
Furthermore, the conversation around testosterone replacement therapy (TRT) highlights a critical disconnect. While TRT can offer benefits for men with clinically low testosterone and associated symptoms, its increasing use in younger men for non-medical reasons carries significant risks. Dr. Eisenberg explains that exogenous testosterone suppresses the body's natural production of both testosterone and sperm, potentially leading to infertility. This underscores the need for careful patient selection and a thorough understanding of the long-term consequences, especially for men of reproductive age. The art of medicine, as Dr. Hyman notes, lies in optimizing lifestyle factors--diet, exercise, sleep, stress management--before considering TRT, as these foundational elements can naturally boost testosterone and improve overall health.
Actionable Strategies for Enhanced Vitality and Fertility
The insights from this conversation offer a clear roadmap for men seeking to improve their reproductive health and overall vitality. The key lies in understanding that these are not isolated issues but interconnected components of a larger system.
- Prioritize Metabolic Health: Focus on a diet low in sugar and refined carbohydrates, and engage in regular exercise, including strength training, to manage weight and reduce belly fat. This directly supports testosterone production and improves sperm quality.
- Minimize Environmental Exposures: Actively reduce contact with endocrine disruptors by opting for organic foods when possible, avoiding plastics for food storage and heating, and choosing personal care products with fewer synthetic chemicals.
- Protect Scrotal Health: Avoid prolonged exposure to heat from hot tubs, saunas, and laptops on the lap. If cycling, opt for designs that reduce pressure and heat, and stand up periodically.
- Manage Lifestyle Factors: Moderate alcohol consumption, prioritize 7-9 hours of quality sleep, and implement stress-reduction techniques such as meditation or breathwork.
- Consider Targeted Supplementation: Explore scientifically backed supplements that support sperm health, mitochondrial function, and cellular repair, such as antioxidants, CoQ10, omega-3s, and specific nutrients like zinc and spermidine.
- Get Comprehensive Health Testing: Beyond basic check-ups, advocate for testing of key hormones (total and free testosterone, estradiol, prolactin, LH) and other biomarkers to gain a full understanding of hormonal balance and metabolic health.
- Be Cautious with Testosterone Therapy: For men of reproductive age, carefully weigh the risks and benefits of TRT with a healthcare provider, prioritizing lifestyle optimization and exploring fertility-preserving alternatives if conception is a goal.
- Embrace Proactive Health Monitoring: View semen analysis not just as a fertility test but as a valuable indicator of overall health and longevity, prompting early intervention and lifestyle adjustments.
- Educate and Advocate: For women, encourage male partners to prioritize their health and seek comprehensive evaluations. For all men, recognize that reproductive health is a critical component of overall well-being and longevity.