Cholesterol Narrative Flawed; Inflammation and Insulin Resistance Drive Heart Disease
The cholesterol narrative for heart disease is fundamentally flawed, and clinging to it blinds us to the true drivers of cardiovascular illness. This conversation reveals that focusing solely on LDL cholesterol misses the mark for the vast majority of people experiencing heart attacks, leading to ineffective treatments and a continued epidemic. Those who understand the interconnectedness of inflammation, insulin resistance, and metabolic health--and know the right biomarkers to track--gain a significant advantage in proactively safeguarding their long-term well-being. This analysis is crucial for anyone seeking a more accurate and actionable approach to heart health than the conventional, outdated medical dogma.
The Unseen Architect of Heart Disease: Beyond Cholesterol
For decades, the prevailing wisdom on heart disease has been a singular, seemingly straightforward message: cholesterol is the enemy, and lowering LDL is the ultimate goal. This dogma, deeply ingrained in medical training and public perception, has led to a widespread reliance on statins and a general avoidance of dietary fat. However, as Dr. Mark Hyman compellingly argues in this episode of Office Hours, this simplistic view is not only incomplete but actively misleading, obscuring the more complex, interconnected systems that truly drive cardiovascular illness for most individuals. The hidden consequence of this narrow focus is a healthcare system and a public that are largely misdirected, treating symptoms while ignoring root causes.
The most striking revelation is the sheer disconnect between the conventional LDL cholesterol metric and actual heart attack incidence. Dr. Hyman highlights a staggering statistic: in a study of 136,000 heart attack patients, a remarkable 75% had LDL levels considered "normal" by conventional standards. This single data point shatters the illusion that LDL alone is the primary culprit. It suggests that the medical establishment has been fixated on a proxy, a bystander, rather than the actual instigators of arterial damage.
"If cholesterol were truly the main cause of heart disease, then why do people who have heart attacks have normal LDL levels?"
This question, posed by Dr. Hyman, is the pivot point for understanding the deeper dynamics at play. The conventional model fails because it doesn't account for the nuanced nature of cholesterol itself--its particle size, density, and number--nor does it acknowledge the systemic factors that lead to its problematic deposition in arteries. Instead of a simple cause-and-effect relationship between high LDL and heart attacks, the reality is far more intricate, involving inflammation and metabolic dysfunction.
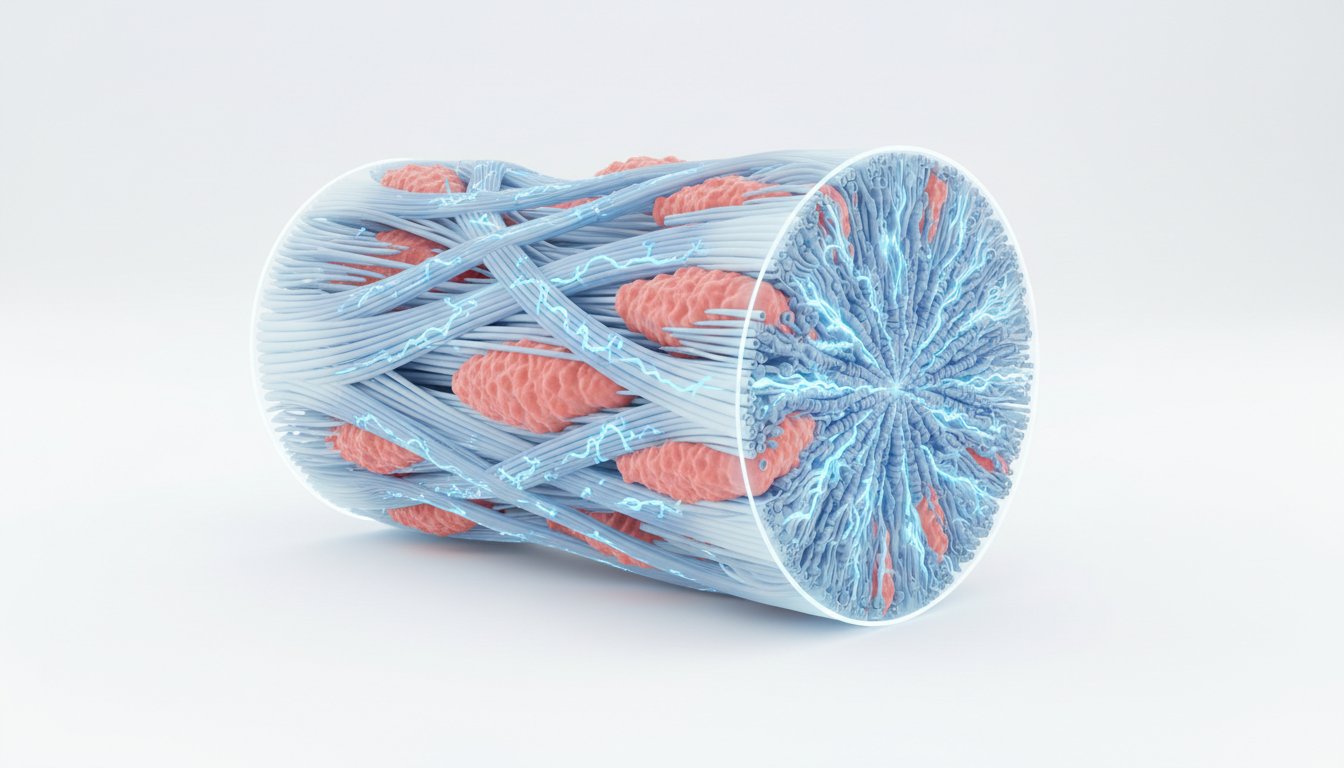
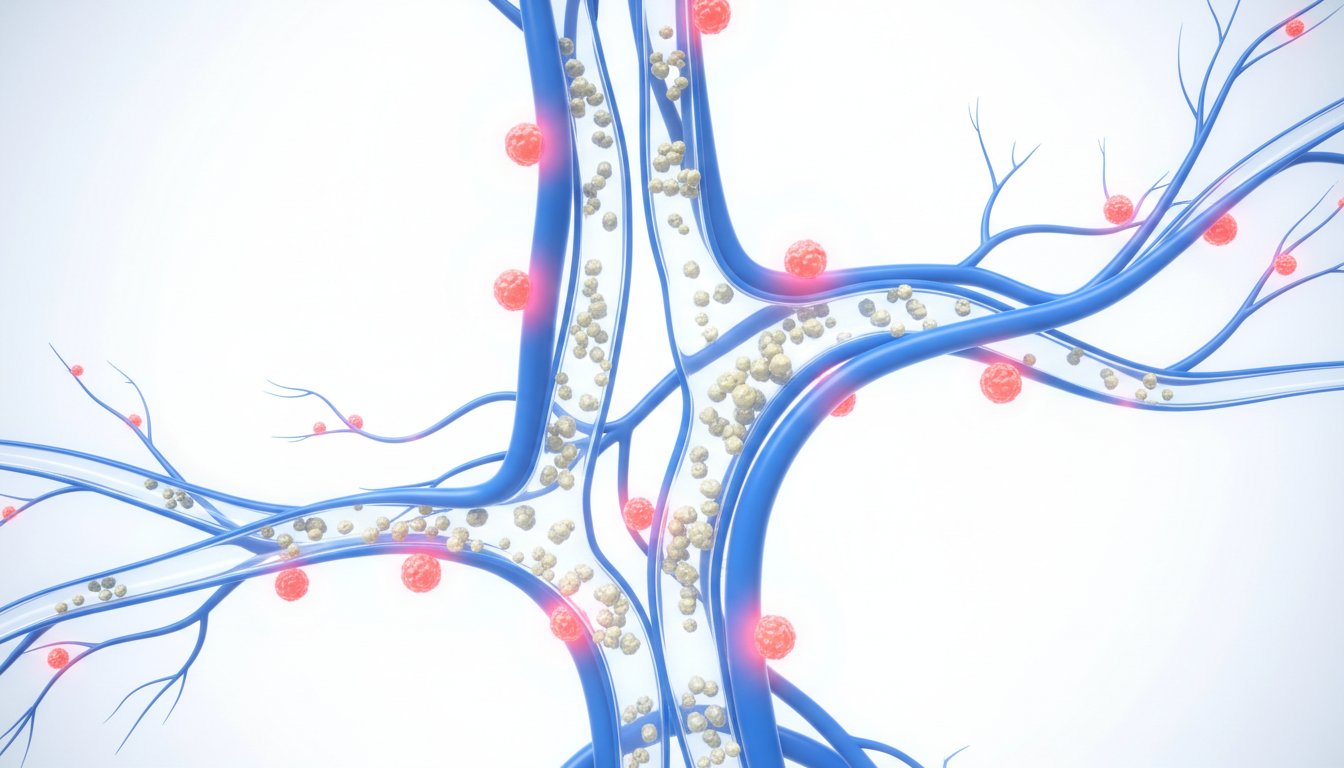
The science that has emerged since Dr. Hyman’s medical training points to inflammation as a more critical factor. Research, notably from Harvard, indicates that high inflammation levels, even with normal cholesterol, can significantly elevate heart disease risk. This shifts the focus from a lipid-centric view to an inflammatory one. But what fuels this inflammation? The answer, often overlooked, is metabolic dysfunction, particularly insulin resistance. For the vast majority of people--Dr. Hyman cites a figure of 93.2% of Americans having some degree of metabolic dysfunction--the root cause of arterial plaque buildup isn't just dietary fat, but the overconsumption of sugar and refined starches. This dietary pattern leads to insulin resistance, which in turn drives inflammation and the production of small, dense LDL particles that are far more atherogenic than their larger counterparts.
"The real problem, the real problem causing our epidemic of heart disease, is not a high-fat diet; it's sugar, and it's insulin resistance that results from eating a lot of starch and sugar."
This statement cuts through the decades of anti-fat messaging, reframing the dietary culprits. The implication is profound: while conventional advice has focused on reducing fat intake, the true battle lies in managing carbohydrate intake and improving insulin sensitivity. This requires a fundamental shift in how we approach nutrition and health, moving away from generalized dietary restrictions towards personalized strategies informed by specific biomarkers. The delayed payoff for addressing metabolic health is immense, creating a durable advantage where others continue to struggle with conventional, ineffective approaches.
The conversation also introduces critical biomarkers that offer a more accurate picture of cardiovascular risk than standard cholesterol panels. Apolipoprotein B (ApoB) is highlighted as a superior marker, directly reflecting the number of atherogenic particles. Lipoprotein(a), or Lp(a), is another crucial genetic factor that, when elevated, significantly increases risk, especially in conjunction with other metabolic issues. The triglyceride-to-HDL ratio is presented as a simple yet powerful indicator of insulin resistance. These markers, often ignored by mainstream medicine, provide the granular data needed to understand the quality and risk profile of one's cardiovascular system, not just the quantity of cholesterol.
"You wouldn't ding a prescription without knowing the problem, right? But that's how most people approach nutrition. They try keto, paleo, plant-based, fasting, just hoping something sticks. In my practice, I've seen it over and over: diet isn't the issue, it's the missing data."
This quote underscores the systemic failure of a data-deficient approach. The conventional wisdom, by not testing for these key indicators, sets individuals up for failure. It’s akin to trying to fix a car without knowing which part is broken. The advantage lies with those who embrace a data-driven, systemic approach, understanding that true health is built on a foundation of accurate biological information and interventions that address the root causes of disease, not just the superficial symptoms. This requires patience and a willingness to look beyond the obvious, to invest in understanding the complex interplay of factors that govern our health, a strategy that pays dividends in long-term vitality.
Key Action Items
- Immediate Action (Within 1-2 weeks):
- Request comprehensive cardiovascular lab tests, including ApoB, Lp(a), hs-CRP, fasting insulin, and triglyceride-to-HDL ratio. If your doctor won't order them, explore direct-to-consumer options.
- Calculate your triglyceride-to-HDL ratio and assess your waist circumference as immediate indicators of metabolic health.
- Significantly reduce or eliminate added sugars and refined starches from your diet. Focus on whole, unprocessed foods.
- Short-Term Investment (1-3 Months):
- Consider using a continuous glucose monitor (CGM) for a period to understand how specific foods impact your blood sugar and insulin response.
- Incorporate regular exercise, including both strength training and cardiovascular activity, into your routine to improve insulin sensitivity and build muscle.
- Prioritize stress management techniques (e.g., mindfulness, meditation) and ensure adequate, quality sleep, as these directly impact inflammation and metabolic health.
- Medium-Term Investment (6-12 Months):
- Track your lab markers regularly (e.g., twice a year) to monitor progress and adjust your interventions based on data.
- Explore high-quality Omega-3 supplements, CoQ10, and magnesium, if indicated by your health status and after consulting with a healthcare professional.
- Consider a baseline calcium score or other imaging to assess existing plaque buildup, providing a more direct measure of arterial disease than cholesterol numbers alone. This investment pays off by offering clarity on actual disease presence, guiding more precise interventions.