Chronic Disease Driven by Processed Foods and Flawed Medicine
The bitter truth about sugar and ultra-processed food is that they are not merely dietary choices but insidious drivers of chronic disease, masquerading as sustenance. This conversation with Dr. Robert Lustig reveals the hidden consequences of our modern food environment: not just weight gain, but a systemic poisoning of our cellular machinery, leading to a cascade of metabolic dysfunctions that medicine, in its current symptomatic approach, fails to address. Those who understand this can gain a significant advantage by focusing on the root causes of health, protecting themselves and their families from the escalating epidemic of chronic illness.
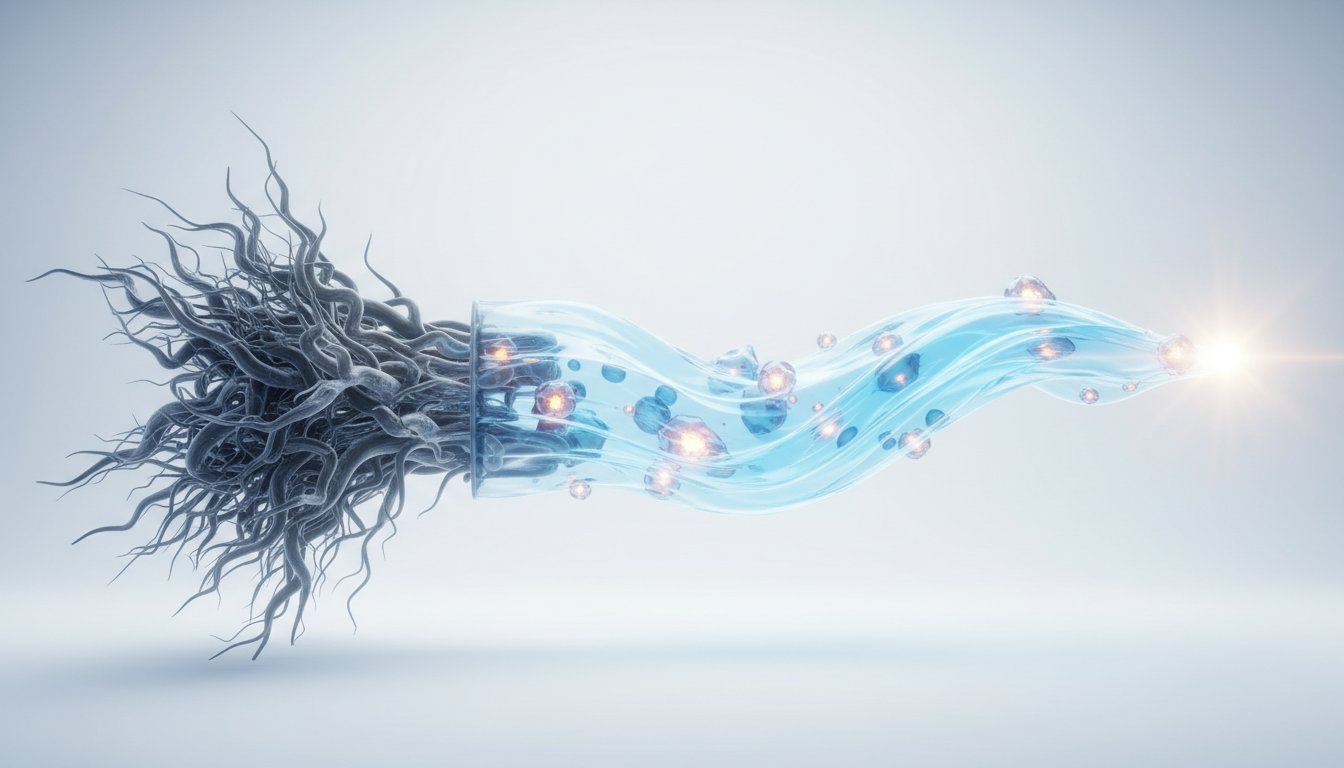
The Mitochondrial Poison: How Sugar Undermines Energy Production
The prevailing narrative around sugar often frames it as simple energy. However, Dr. Robert Lustig argues this is a dangerous oversimplification, akin to calling cyanide "energy" because it can be combusted. In reality, sugar acts as a poison to our mitochondria, the powerhouses of our cells. It disrupts three critical enzymes--AMP kinase, ACADL, and CPT1--essential for energy production and fat oxidation. This isn't just about feeling sluggish; it's about actively inhibiting the body's ability to generate ATP, the fundamental chemical energy currency.
"In other words, when you consume sugar, you are poisoning your mitochondria. You are generating less of the chemical energy that our cells get powered by, called ATP. So if you're making less ATP, is that energy? It's the opposite of energy."
This fundamental disruption of cellular energy production is not a minor inconvenience; it is the bedrock upon which many chronic diseases are built. The food industry, by promoting sugar as energy and ultra-processed foods (UPFs) as "food," has created a system where widespread metabolic dysfunction is not an anomaly but the norm. Lustig posits that UPFs, making up over half of the UK diet, are not food at all, as they fail to contribute to either growth or burning in an organism. Studies, like one by Dr. Kevin Hall at the NIH, show that UPFs lead to increased weight gain and decreased energy expenditure compared to real food, even when calories are controlled. This directly contradicts the "eat less, move more" mantra, suggesting that the type of food is more critical than simply its caloric content.
The Liver's Overload: Sugar's Alcohol-Like Assault
The comparison between sugar and alcohol is not hyperbole; it's a functional parallel. Just as the liver metabolizes alcohol, it processes fructose, a primary component of sugar. While the intestine can divert a small amount of sugar away from the liver through de novo lipogenesis (converting sugar to fat in the intestine), this capacity is easily overwhelmed. When this happens, the excess fructose floods the liver, initiating the same damaging processes as alcohol: glycation, oxidative stress, mitochondrial dysfunction, and insulin resistance.
This liver-centric damage is particularly insidious because it underpins a host of chronic diseases, including type 2 diabetes, heart disease, cancer, and Alzheimer's. The pancreas responds to this hepatic dysfunction by producing more insulin, leading to systemic insulin resistance. Lustig's "aha moments" reveal the depth of this understanding: his work with hypothalamic obesity showed that insulin, not just caloric intake, drives weight gain, and that treating insulin resistance could reverse symptoms and improve quality of life.
"The problem with sugar in the liver is exactly the same as the problem of alcohol in the liver because it causes the exact same processes. It causes glycation, it causes oxidative stress, it causes mitochondrial dysfunction, and basically drives insulin resistance."
This insight challenges the conventional medical approach, which often treats symptoms downstream--managing diabetes with oral hypoglycemics or hypertension with statins--without addressing the root cause: the overloaded liver and systemic insulin resistance driven by dietary sugar.
The Deception of the Scale: TOFI and Hidden Fat
The common reliance on the scale as the arbiter of health is a critical flaw in our understanding. Dr. Lustig introduces the concept of TOFI (Thin On The Outside, Fat On The Inside), highlighting that visible fat is only one part of the story. He identifies three distinct fat depots, each with different health implications:
- Subcutaneous Fat: The fat we can see (e.g., on the thighs and buttocks). While potentially cosmetically undesirable, it is largely metabolically inert and has a high capacity to store energy before becoming problematic. It takes approximately 22 pounds of excess subcutaneous fat before significant health issues arise.
- Visceral Fat: The stress-related fat around the abdomen. This fat is metabolically active and drains directly into the liver via the portal vein. Even a small amount, around 5-6 pounds, can generate enough inflammatory cytokines to cause liver damage and insulin resistance. This is often linked to chronic stress and cortisol.
- Liver Fat: Fat stored within the liver itself. This is the most egregious, as it directly impairs liver function. As little as half a pound of liver fat can lead to metabolic dysfunction and insulin resistance. This is primarily driven by sugar consumption through de novo lipogenesis.
The critical takeaway is that individuals can appear thin externally while harboring significant visceral and liver fat, leading to TOFI. This explains why an alarming 88% of Americans exhibit some degree of metabolic dysfunction, often without realizing it because the scale doesn't tell the whole story. The insidious accumulation of liver fat, driven by sugar, is a silent epidemic affecting even children, with 20% of children showing liver fat unrelated to obesity.
Modern Medicine's Symptom-Centric Approach: The Leaking Roof Analogy
Dr. Lustig is highly critical of modern medicine's tendency to treat symptoms rather than root causes. He likens it to playing a game of "Clue," matching symptoms to diagnoses and treatments without addressing the underlying mechanisms. The "hateful eight"--glycation, oxidative stress, mitochondrial dysfunction, insulin resistance, membrane instability, inflammation, methylation issues, and autophagy problems--are the true root causes of chronic diseases like type 2 diabetes, hypertension, cardiovascular disease, cancer, and dementia. These eight processes, when out of balance, lead to the diseases we commonly recognize, but medicine often focuses on managing the downstream manifestations (e.g., prescribing statins for dyslipidemia) rather than fixing the fundamental issues.
"You have to work upstream of a problem to solve a problem. Working downstream of a problem only fixes the result of the problem. The problem's still there."
This "leaking roof" analogy perfectly encapsulates the issue: buckets (medications) collect the water (symptoms), but the leak (the root cause) remains unaddressed. Until we fix the leak--by addressing diet and metabolic health--we will continue to be inundated by chronic disease. This is why Lustig advocates for "insulin reduction clinics," focusing on lowering insulin levels as a primary strategy to combat metabolic dysfunction.
Actionable Takeaways for Health and Longevity
- Prioritize Real Food: Actively reduce consumption of ultra-processed foods. Focus on foods that your grandparents would recognize as food, ideally with fewer than five ingredients.
- Protect the Liver: Significantly limit sugar intake, especially from sugar-sweetened beverages and refined carbohydrates. Understand that fructose directly impacts liver health.
- Feed the Gut: Increase intake of dietary fiber from whole foods. Fiber is crucial for gut bacteria, which play a vital role in inflammation, insulin sensitivity, and even mood regulation.
- Be Wary of "Diet" Options: Diet drinks, while calorie-free, can disrupt metabolic signaling, increase appetite, alter the gut microbiome, and potentially promote fat deposition. Opt for water or unsweetened beverages.
- Understand Fat Beyond Weight: Recognize that visceral and liver fat are metabolically dangerous, even if you appear thin. Consider getting blood tests to assess metabolic health markers beyond just body weight.
- Children are Canaries: Be extremely vigilant about sugar and processed food intake in children. It can lead to early liver fat accumulation, behavioral changes, and set the stage for lifelong chronic disease.
- Focus on Root Causes: Advocate for and adopt a health approach that addresses the underlying metabolic dysfunction (like insulin resistance and mitochondrial health) rather than just managing symptoms.
- Short-Term Discomfort for Long-Term Gain: Embracing a real-food diet may involve initial challenges and discomfort as your body adjusts and you navigate a food environment that promotes UPFs. This effort, however, yields significant long-term health advantages and a greater capacity to "feel better and live more."