Inflammation and AI Replace Clogged Arteries in Heart Attack Prevention
The traditional "plumbing" model of heart attacks, focused on clogged arteries, is being replaced by a more nuanced understanding of inflammation and plaque instability. This shift, driven by new technologies like AI-powered CT scans and advanced blood markers, promises a proactive approach to prevention. The non-obvious implication is that many individuals previously considered "low risk" may actually be in danger, while those with known risk factors can be managed with unprecedented precision. This conversation reveals the hidden consequences of outdated medical paradigms and offers a glimpse into a future where personalized, data-driven interventions can preemptively neutralize threats before they manifest as catastrophic events. Healthcare providers, researchers, and patients alike stand to gain a significant advantage by embracing this evolving science, moving beyond symptom management to true disease prevention.
The Inflammation Cascade: Beyond Blockages to Vulnerability
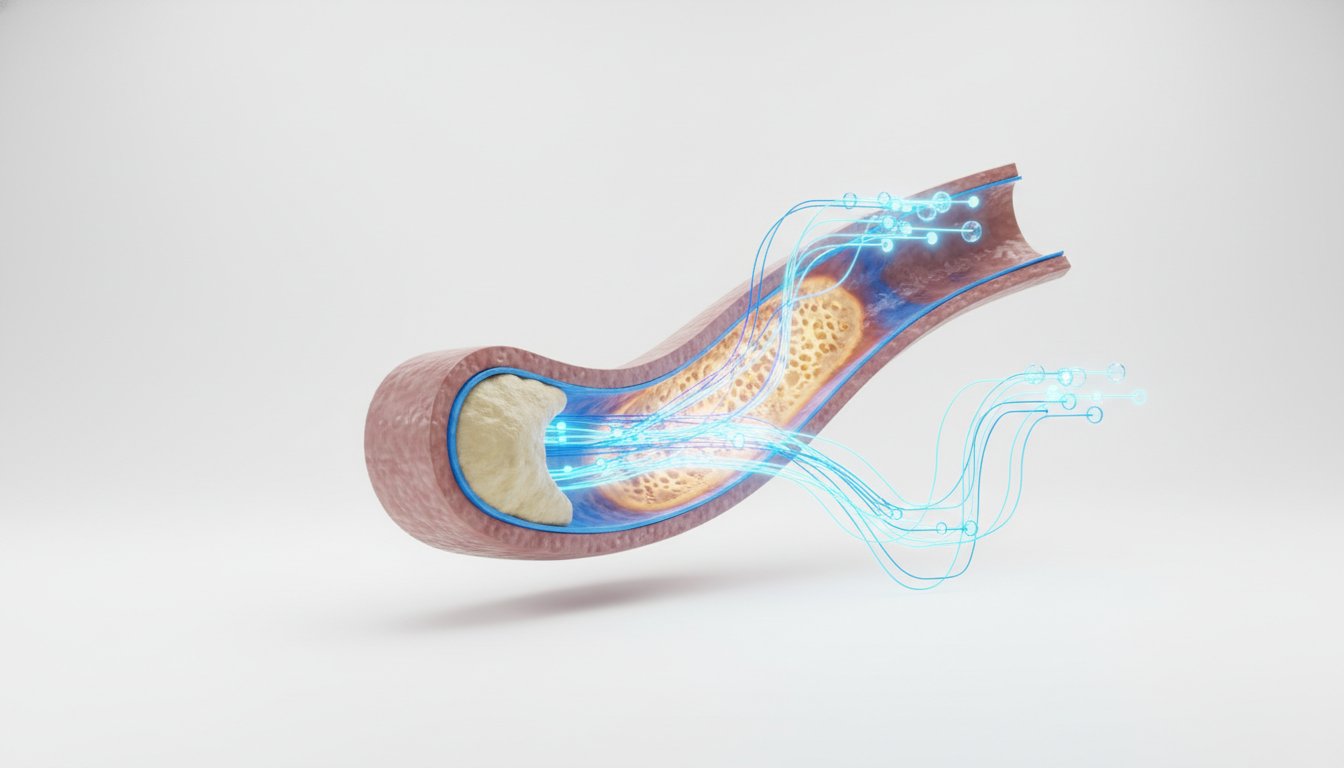
For decades, the prevailing narrative around heart attacks was one of simple mechanical failure: arteries clogged with fatty plaque, akin to pipes accumulating gunk. The primary diagnostic and therapeutic focus was on the degree of narrowing, the visible obstruction. However, as cardiologist Eric Topol explains, this "plumbing" model proved insufficient. A significant number of heart attacks occurred in individuals with seemingly clear arteries, a discrepancy that pointed to a deeper, more insidious process.
"Heart disease is still the biggest killer in the world, but in the past few years, a bunch of new technologies have come together, and it seems like a new, better approach to preventing heart attacks may be here very soon."
This realization marked a pivotal shift, moving the focus from the quantity of plaque to its quality--specifically, its inflammatory state. The new paradigm recognizes that even a small amount of plaque can be dangerous if it's inflamed, unstable, and prone to rupture. This instability is the direct precursor to the clot formation that causes a heart attack. The implications are profound: a person might have "clean pipes" but still be at high risk due to underlying inflammation. This reorientation means that identifying and mitigating inflammation is now central to preventing heart attacks.
The AI-Augmented Artery Scan: Unmasking Silent Inflammation
A key technological advancement enabling this shift is the combination of CT scans of the heart's arteries with Artificial Intelligence. This synergy allows for the detection of inflammation, a critical risk factor that was previously invisible. A study in the UK involving 40,000 people demonstrated the power of this approach: individuals with inflamed arteries, even without significant narrowing, showed a dramatically elevated risk of heart attack and death.
"If you have all three arteries inflamed, the risk ratio for having a heart attack over the next few years is like 30-fold. I mean, a huge increase. If one artery is inflamed, it's still important. So we have now moved in the whole dogma of cardiology from blockages to inflammation."
This AI-driven analysis, soon to be FDA-approved via companies like Caristo, represents a move towards "autodidactic" learning--allowing data to reveal patterns without human bias. The AI, trained on vast datasets, can identify subtle indicators of inflammation that might be missed by human eyes. This technology offers a non-invasive way to map a patient's arterial health, providing a much clearer picture of their true risk than traditional methods. The advantage for patients and clinicians is a more precise identification of who needs intervention, moving beyond broad risk categories to individual vulnerability.
The Multi-Omic Stack: A Holistic View of Risk
Once high risk is identified, the next challenge is effective intervention. This involves a comprehensive approach that goes far beyond simply lowering LDL cholesterol, though achieving very low LDL levels (below 20 or 10 in high-risk individuals) remains important. The new science integrates multiple data points--a "stack" of information--to create a personalized risk profile and treatment plan. This includes measuring Lipoprotein(a) [Lp(a)], a genetic risk factor for which new treatments are emerging.
Inflammation markers, such as high-sensitivity C-reactive protein (hs-CRP), are also crucial. But the concept of inflammation itself is being refined. It's understood as a complex immune response to injury, which, in arteries, can become a self-perpetuating cycle. This chronic inflammation can lead to plaque rupture and subsequent clot formation. Beyond these, emerging tools like "artery clocks," "heart clocks," and "immune system clocks"--collections of proteins in the blood that indicate organ aging--provide further insights into an individual's biological risk.
The integration of these markers, alongside lifestyle factors like sleep and exercise, creates a dynamic picture. This multimodal approach, powered by AI, can predict not just if someone is at risk, but when they might have a heart attack, allowing for timely and targeted interventions. The ability to track changes in these markers in response to interventions--be it lifestyle changes, medication, or other therapies--provides a feedback loop that was previously unimaginable.
The Unforeseen Power of GLP-1 Drugs: Beyond Weight Loss
Perhaps one of the most surprising developments is the impact of GLP-1 receptor agonist drugs, commonly known for weight loss. While their efficacy in reducing weight is well-established, a significant finding from clinical trials revealed that a substantial portion of their cardiovascular benefit is not due to weight loss. This suggests a more direct anti-inflammatory mechanism at play.
"The biggest story about this family of drugs is that their, their main mechanism of action, well, the cosmetic and other health benefits of carrying lesser weight, that's great. But their big, their big impact is to lower total body and brain inflammation."
These drugs appear to directly influence the immune system and the brain, both key regulators of inflammation. By interacting with GLP receptors on immune cells and in the brain, they can effectively dampen the inflammatory cascade. This finding opens a new frontier in anti-inflammatory therapies for cardiovascular disease, potentially offering a more potent and direct approach than statins, which primarily target LDL cholesterol. The implications are vast, suggesting a future where a range of anti-inflammatory strategies, including those targeting inflammasomes and the gut microbiome, will blossom.
Genetic Predisposition and Predictive AI: When and Why
Genetic predisposition, long understood as a factor in heart disease, is now being assessed with greater precision through polygenic risk scores (PRS). These scores analyze hundreds of gene variants to provide a more comprehensive picture of an individual's genetic susceptibility. While PRS can identify high-risk individuals, they historically struggled to predict when a heart attack might occur.
This is where advanced AI models, such as the Delphi 2M model, are revolutionary. By integrating PRS with a vast array of other data--electronic health records, protein markers, CT scans, and even retinal images--these models can predict disease onset with remarkable accuracy, including the timing. The ability to predict when a heart attack might occur, rather than just if, transforms prevention from a reactive strategy to a proactive one. This predictive power, derived from analyzing complex, multimodal data that humans cannot process alone, is a testament to AI's role in the future of medicine.
Key Action Items
- Immediate Action: Discuss your personal heart attack risk with your doctor, inquiring about advanced screening methods like CT angiography with AI-driven inflammation detection.
- Immediate Action: If you have a family history of heart disease or other risk factors, explore genetic testing for polygenic risk scores, which are becoming increasingly accessible and affordable.
- Short-Term Investment (0-6 months): Inquire with your physician about current anti-inflammatory medications (e.g., low-dose colchicine) and emerging treatments for Lp(a) if relevant.
- Short-Term Investment (0-6 months): Prioritize sleep hygiene and consistent physical activity, as these are foundational for managing inflammation and overall cardiovascular health.
- Medium-Term Investment (6-18 months): Stay informed about the FDA approval and insurance coverage of new AI-driven diagnostic tools for heart attack risk assessment.
- Medium-Term Investment (6-18 months): Engage in conversations with your healthcare provider about the potential benefits of GLP-1 drugs for cardiovascular risk reduction, independent of weight loss, if appropriate for your health profile.
- Long-Term Investment (12-24 months+): Advocate for the integration of comprehensive multi-omic data analysis (genetics, proteins, scans, lifestyle) into routine cardiovascular care, leveraging AI for personalized risk prediction and intervention timing.