Dietary Interventions Improve Mitochondrial Function for Mental Health
TL;DR
- Mental disorders are fundamentally metabolic in nature, with diet being a critical factor that can contribute to the current mental health epidemic and offer a path to healing.
- Ultra-processed foods with artificial chemicals can cause mitochondrial dysfunction, mirroring the cellular damage seen after trauma and leading to a cascade of mental health issues.
- The ketogenic diet, originally developed for epilepsy, can induce profound remission in severe mental illnesses like schizophrenia by improving mitochondrial function and reducing brain inflammation.
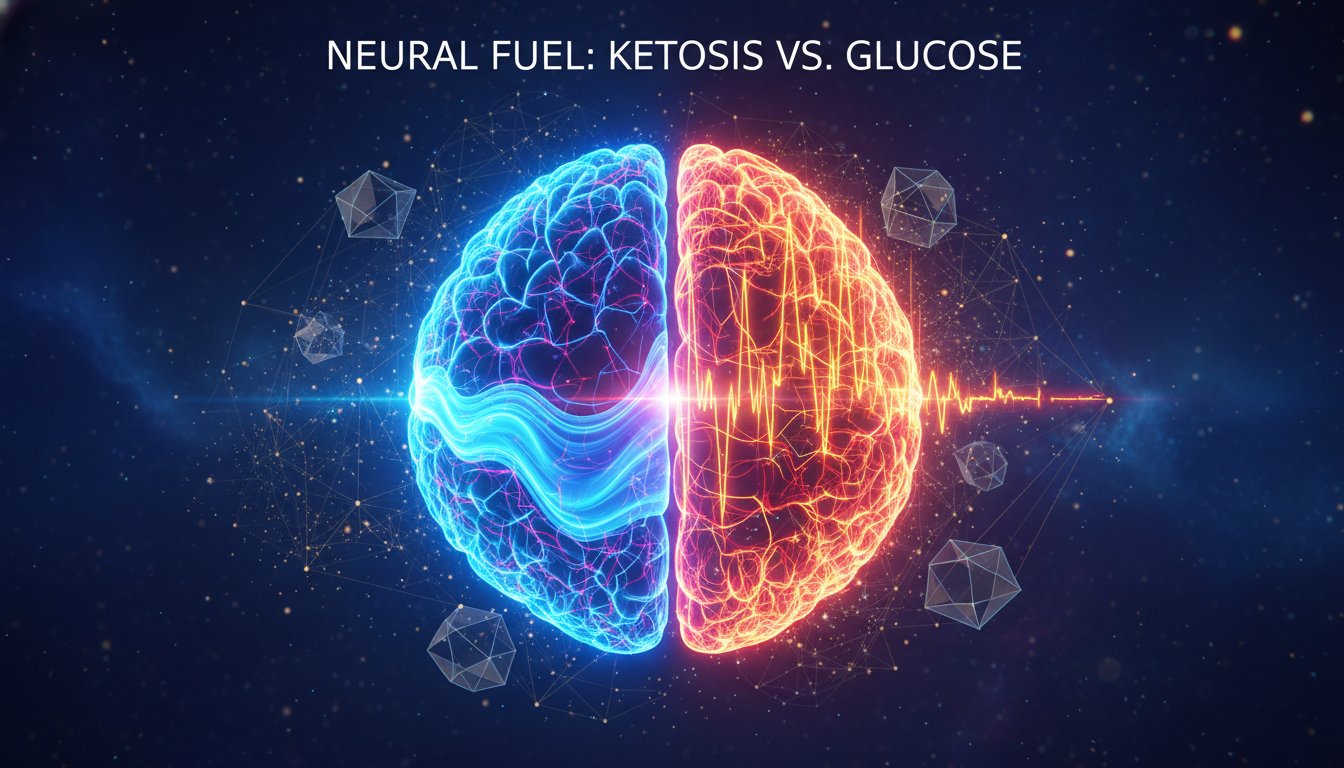
- Fasting and ketogenic diets mimic each other's beneficial effects on mitochondrial biology, neurotransmitters, and insulin signaling, offering therapeutic potential for brain health.
- High sugar intake over time dysregulates glucose levels, leading to mitochondrial dysfunction and oxidative stress, which is a unifying theme across metabolic and mental disorders.
- Weight gain, particularly around puberty, significantly increases the risk of developing depression, while insulin resistance in childhood dramatically elevates the likelihood of psychotic disorders.
Deep Dive
Mental disorders are fundamentally metabolic in nature, with diet playing a critical, yet widely disregarded, role in their development and potential resolution. This perspective challenges conventional psychiatric approaches, suggesting that improving mitochondrial function through dietary changes can offer a powerful pathway to healing chronic and debilitating mental illnesses.
The causal chain from diet to mental health is rooted in mitochondrial function. Modern, ultra-processed foods, often high in sugar and containing artificial compounds, can lead to mitochondrial dysfunction. This dysfunction creates oxidative stress, a known contributor to metabolic disorders and mental health conditions. For instance, high sugar intake dysregulates glucose levels, directly impairing mitochondria. This metabolic disruption is a unifying factor across a spectrum of conditions, from obesity and diabetes to anxiety, depression, bipolar disorder, and even schizophrenia, all of which are associated with increased risks of Alzheimer's disease. Epidemiological studies and animal models demonstrate a clear link between diets high in ultra-processed foods and increased rates of depression and anxiety. When mitochondria function poorly, the body's ability to produce energy efficiently is compromised, leading to a cascade of negative effects that manifest as mental health symptoms.
Dietary interventions, particularly those that mimic fasting states, show significant promise. The ketogenic diet, originally developed to treat epilepsy, has demonstrated remarkable efficacy in treating severe mental illnesses. A case study of "Doris," diagnosed with schizophrenia, illustrates this potential: after adopting a ketogenic diet for weight loss, her hallucinations and delusions remitted within weeks, leading to a complete cessation of psychiatric medication and symptoms for the remaining 15 years of her life. This suggests the ketogenic diet, by forcing the body to produce ketone bodies, fundamentally alters brain and body metabolism and improves mitochondrial function, reducing inflammation and changing gene expression. Fasting, which the ketogenic diet mimics, offers similar benefits by enhancing mitochondrial biology and improving insulin signaling.
The implications are profound: a significant majority of the population (93%) exhibits signs of metabolic health problems, indicating widespread vulnerability to diet-related mental health issues. While conventional psychiatry often overlooks diet, a metabolic approach, focusing on mitochondrial health through interventions like the ketogenic diet or supervised fasting, offers a powerful, evidence-based strategy for recovery from severe mental illness, challenging the notion that such conditions are solely rooted in psychological or genetic factors.
Action Items
- Implement dietary audit: Track 7-day food intake for 3-5 individuals to identify ultra-processed food consumption patterns.
- Create educational material: Draft a 1-page summary on mitochondrial dysfunction and its link to mental health, targeting 5 key takeaways.
- Evaluate personal diet: Analyze current food intake against low-carbohydrate and ketogenic principles for potential metabolic health improvements.
- Track 3-5 metabolic health biomarkers: Monitor blood pressure, blood glucose, and lipid profiles over a 3-month period to assess dietary impact.
Key Quotes
"If you delve into the science -- all the accumulated research from the last 100 years and beyond, including neuroimaging, genetic, neurotransmitter, hormone, trauma, and adverse childhood experiences studies -- and understand what's happening in the brains and bodies of people as a consequence of these factors, you arrive at one conclusion: mental disorders are metabolic in nature. It is incontrovertible that diet plays a massive role in metabolism. Therefore, I strongly believe that diet might be contributing to the mental health epidemic we're witnessing, and it also might offer a path to hope, healing, and recovery. As a scientist and clinician, I know with certainty that diet can heal and help people recover from chronic, horrible, debilitating mental illnesses."
Dr. Palmer argues that a comprehensive review of scientific research leads to the conclusion that mental disorders are fundamentally metabolic. He asserts that diet is a critical factor in metabolism, suggesting it contributes to the current mental health crisis and offers a potential avenue for recovery. Dr. Palmer states with certainty, based on his scientific and clinical experience, that dietary changes can lead to healing from severe mental illnesses.
"From my own personal story, during medical school and residency, I suffered from low-grade depression, OCD, and other symptoms. I also developed metabolic syndrome, including high blood pressure, high cholesterol, and pre-diabetes. I wasn't significantly overweight and was exercising, but I was following a low-fat diet, mostly of processed foods because they were cheaper. This was the diet touted as healthy at the time -- low in fat was supposedly good for us. My metabolic syndrome continued to worsen. To treat it, I changed my diet to a low-carbohydrate one. Within three months, my metabolic syndrome was completely gone. What truly dumbfounded me was that my mental health was better than it had ever been in my entire life."
Dr. Palmer shares his personal experience of suffering from depression and metabolic syndrome while adhering to a low-fat, processed food diet. He explains that switching to a low-carbohydrate diet resolved his metabolic issues and, unexpectedly, significantly improved his mental health. This personal narrative serves as an example of how dietary changes can have profound effects on both physical and psychological well-being.
"But if I have that profile, if I have that sort of mental health profile now, as I sit here, and then for the next decade I eat processed junk food, am I going to send my mitochondria into disarray, which is going to increase the probability that I have a mental health disorder? Yes, I think yes. We have, you know, there's no way we will ever be able to do a human randomized controlled trial to test that precise, unethical hypothesis. But we have large epidemiological studies that strongly suggest that people who eat a lot of ultra-processed food have a higher risk for developing depression, anxiety, and other mental disorders."
Dr. Palmer responds affirmatively when asked if a diet of processed junk food could lead to mitochondrial dysfunction and an increased risk of mental health disorders. He acknowledges the ethical impossibility of conducting a direct human trial for this hypothesis but points to large epidemiological studies. These studies, Dr. Palmer notes, indicate a strong correlation between high consumption of ultra-processed foods and an elevated risk of developing conditions like depression and anxiety.
"So, one story that I will just share, just because it's probably one of the most powerful stories I know, was a woman whose real name was Doris. In the book, I called her Mildred because I changed everybody's names, but she actually gave me permission to use her real name, so in honor of her, I want to use her real name. She was a woman who actually had a horrible, abusive childhood, lots of trauma. And by the time she turned 17, she started having daily hallucinations and delusions and was diagnosed with schizophrenia. Over the ensuing decades, she tried numerous antipsychotics, mood stabilizers, antidepressants, and other medicines, but none of them stopped her symptoms. She remained with all of the symptoms of schizophrenia. She ended up gaining a massive amount of weight. She ended up weighing about 330 pounds. By the time she was 70, her life was devastated by this diagnosis."
Dr. Palmer introduces the case of Doris, a woman diagnosed with schizophrenia at age 17 who experienced decades of persistent symptoms despite trying various psychiatric medications. He details how her condition led to significant weight gain, reaching 330 pounds by age 70, and how her life was severely impacted by the diagnosis. Dr. Palmer uses Doris's story to illustrate the potential limitations of conventional treatments for severe mental illness and to set the stage for discussing alternative interventions.
"So, unbeknownst to most people, the ketogenic diet was developed over 100 years ago now by a physician for one and only one purpose: it was developed to stop seizures. And in fact, the ketogenic diet has been studied extensively for its effects on the brain over the past 100 years, and it is an evidence-based treatment for epilepsy. And the reason that that is so important is because we use epilepsy treatments in psychiatry all the time. Lots of the medications that we prescribe to psychiatric patients are in fact epilepsy treatments. And so we know that there's a lot of overlap between epilepsy and mental illness, and that treatments that help with epilepsy can also help with mental illness."
Dr. Palmer explains that the ketogenic diet, often perceived as a fad, was originally developed over a century ago specifically to treat seizures. He highlights that its efficacy for epilepsy is well-documented through extensive research on its brain effects. Dr. Palmer emphasizes the relevance of this to psychiatry, noting that many psychiatric medications are also used to treat epilepsy, suggesting a significant overlap in the underlying biology and a potential for epilepsy treatments to benefit mental illness.
"But at the end of the day, I'm convinced that it's really the metabolic changes and the mitochondrial changes that are so important and that are so instrumental in these dramatic improvements in things like stopping seizures or stopping hallucinations and delusions."
Dr. Palmer expresses his conviction that the profound improvements observed in conditions like seizures, hallucinations, and delusions are primarily driven by metabolic and mitochondrial changes. He believes that the ketogenic diet's effectiveness stems from its ability to induce these fundamental shifts in the body's energy processing and cellular function. Dr. Palmer posits that these metabolic and mitochondrial alterations are the key mechanisms behind the dramatic recoveries seen in patients.
Resources
External Resources
Books
- "Title" by Author - Mentioned in relation to the author's book, specifically chapter four, which discusses the link between ADHD, obesity, and mental health disorders.
Research & Studies
- Neuroimaging studies - Referenced as part of the scientific evidence accumulated over the last 100 years that supports the metabolic nature of mental disorders.
- Genetic studies - Referenced as part of the scientific evidence accumulated over the last 100 years that supports the metabolic nature of mental disorders.
- Neurotransmitter and hormone studies - Referenced as part of the scientific evidence accumulated over the last 100 years that supports the metabolic nature of mental disorders.
- Trauma studies - Referenced as part of the scientific evidence accumulated over the last 100 years that supports the metabolic nature of mental disorders.
- Adverse childhood experiences studies - Referenced as part of the scientific evidence accumulated over the last 100 years that supports the metabolic nature of mental disorders.
- Epidemiological studies - Used to suggest that individuals consuming large amounts of ultra-processed food have a higher risk of developing depression and anxiety.
- Animal models (mice and rats) - Used to demonstrate that an obesogenic diet (high in carbohydrates and ultra-processed foods) leads to higher rates of obesity, diabetes, pre-diabetes, depression, and anxiety.
Tools & Software
- Ketogenic diet - Discussed as a dietary intervention for weight loss and its dramatic effects on mental health symptoms, including schizophrenia, hallucinations, and delusions.
Articles & Papers
- "Title" (Source) - Discussed as part of the scientific evidence accumulated over the last 100 years that supports the metabolic nature of mental disorders.
People
- Doris (Mildred) - Case study of a woman with schizophrenia whose symptoms went into remission after adopting a ketogenic diet.
Organizations & Institutions
- Duke University - Mentioned as the location of a weight loss clinic that utilized the ketogenic diet.
Other Resources
- Metabolic syndrome - Discussed as a condition that can be improved by changing diet, with implications for mental health.
- Mitochondria - Central to the discussion of metabolism and its role in mental health, with dysfunction linked to various disorders.
- Metabolism - Identified as the unifying thread connecting metabolic syndrome, mental disorders, and mitochondrial function.
- Oxidative stress - Directly related to mitochondria and linked to metabolic and mental disorders.
- Fight or flight response - Discussed in relation to anxiety and stress responses.
- Epilepsy - Mentioned as a condition where ketogenic diets are an evidence-based treatment, highlighting overlap with mental illness treatments.
- Gut microbiome - Discussed as a factor influenced by diet and fasting, with beneficial changes noted.
- Insulin signaling and insulin resistance - Identified as areas positively impacted by fasting and ketogenic diets.
- Fasting - Discussed as a practice that mimics the fasting state and has beneficial effects on mitochondrial biology, neurotransmitters, and gut microbiome.
- Sugar intake - Discussed in relation to its potential to impair mitochondrial function and contribute to metabolic and mental disorders.