Gut Microbiome's Role in Systemic Inflammation and Health
This conversation with Dr. Will Bulsiewicz reveals a profound, often overlooked truth: the gut microbiome is not merely a passenger in our health but the central command center for our immune system, dictating our experience of inflammation and energy. The non-obvious implication is that many common health struggles, from fatigue to chronic pain, are not isolated events but downstream consequences of a compromised gut barrier, a state exacerbated by modern diets and lifestyles. Individuals seeking to move beyond superficial symptom management and achieve lasting well-being, particularly those struggling with chronic inflammation or low energy, will find this analysis invaluable. By understanding the gut-immune axis, they gain a strategic advantage in addressing the root causes of illness, shifting from a reactive approach to proactive, systemic healing.
The Gut-Immune Axis: Where Your Story Becomes Your Biology
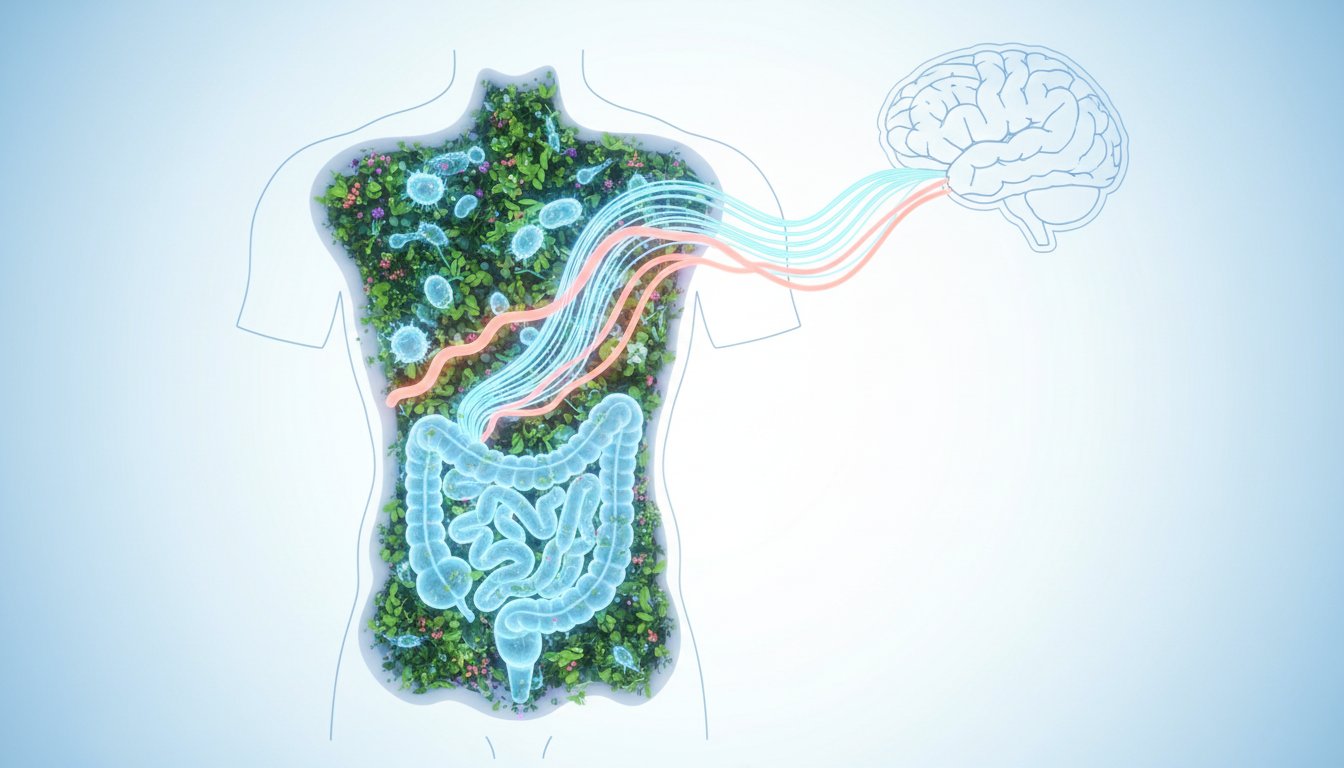
The conventional view of health often compartmentalizes bodily systems, treating inflammation, fatigue, or immune responses as separate issues. Dr. Will Bulsiewicz, however, presents a powerful, interconnected model: the gut and the immune system are inextricably linked, with the gut microbiome acting as the primary architect and regulator of our internal defense mechanisms. This isn't just about digestion; it's about the fundamental architecture of our well-being. The sheer scale of this connection is staggering: 38 trillion microorganisms reside in our gut, outnumbering our own human cells. More critically, 70% of our immune system is housed within the lining of our intestines.
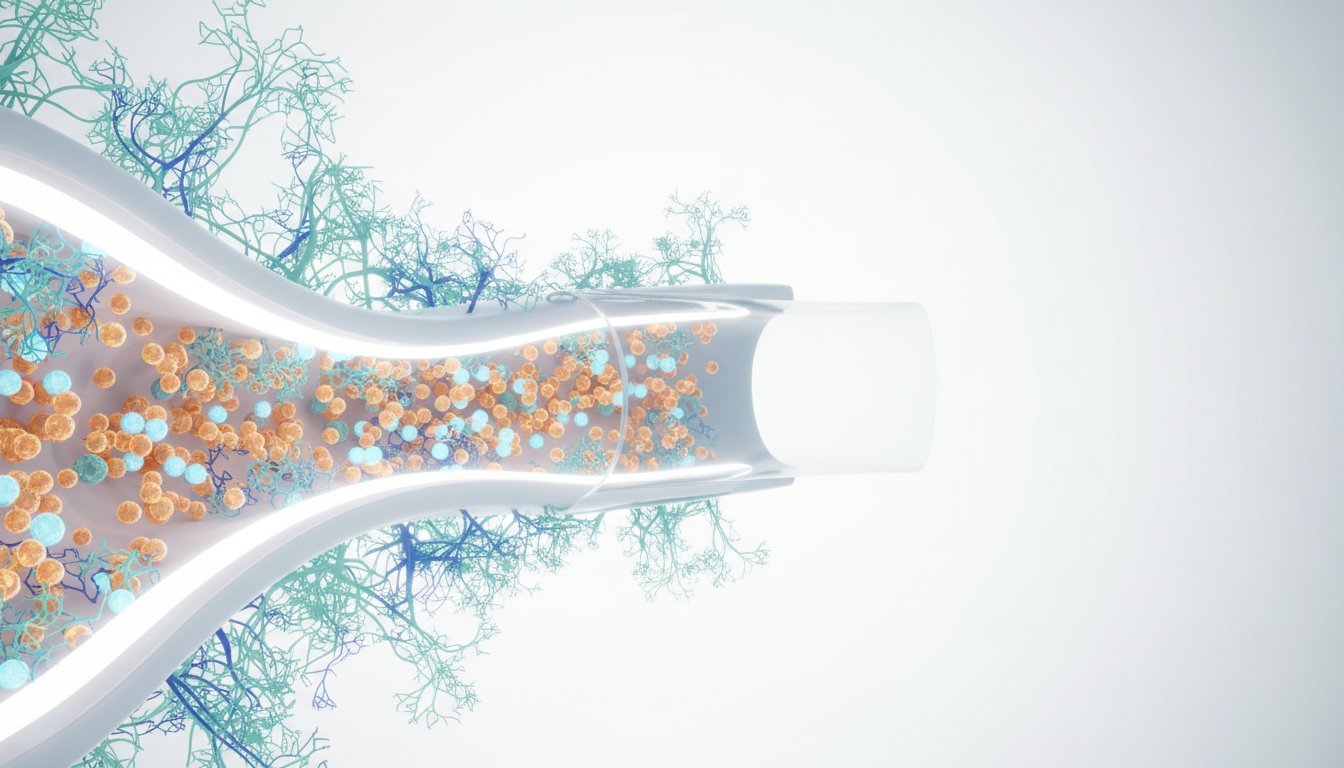
This close proximity means the gut barrier--a single layer of cells--is the crucial interface between the trillions of microbes and our immune cells. When this barrier is strong, fortified by a healthy microbiome that acts as its "steward," the immune system remains at ease. However, modern diets and environmental factors can weaken this barrier, a condition often referred to as "leaky gut" or increased intestinal permeability. When this happens, substances that should remain contained, like lipopolysaccharides (LPS) from the outer armor of certain bacteria, can cross into the bloodstream.
"The gut microbes are the stewards of the gut barrier. They build it for us, they repair it for us."
This breach triggers an immune response. The immune cells, recognizing these foreign invaders, initiate a constant, low-grade battle. This isn't the acute, feverish response to a sudden infection; it's a persistent, internal conflict. Dr. Bulsiewicz likens this to a constant state of war, where the immune system, activated by breaches in the gut barrier, causes what he calls "bodily injury." This chronic inflammation, he notes, is associated with an astonishing number of health conditions--over 130 identified in his research. The immediate problem of a weakened gut barrier thus cascades into widespread systemic issues, demonstrating how a seemingly localized problem can have far-reaching, detrimental effects on overall health.
The Microbiome as a Mirror: Your Life's Narrative in Your Gut
Beyond its role in immunity, the gut microbiome serves as a remarkable biological ledger, reflecting the totality of our lifestyle choices and experiences. Dr. Bulsiewicz emphasizes that the genetic code of our microbiome, derived from our environment and manipulated by our decisions, vastly outweighs our own inherited human DNA--99.5% versus 0.5%. This means that a snapshot of our gut microbes can reveal a detailed story of how we've been living.
"Your life is a story, and that story is actually reflected, it's told through your gut microbiome. So it's entirely unique to you."
The composition of our microbiome is influenced by everything from our food choices and sleep patterns to our exercise habits, stress levels, and even past traumas. This intricate interplay means that our gut isn't just a passive recipient of our actions; it actively encodes them. This has profound implications for how we understand and address health. Instead of viewing symptoms in isolation, we can see them as signals from a microbiome that is communicating the cumulative impact of our life choices. This perspective shifts the focus from merely treating symptoms to understanding and rewriting the narrative written in our gut.
The conventional approach often involves interventions that address immediate symptoms without altering the underlying conditions that led to them. For instance, a quick fix might reduce inflammation temporarily but fail to repair the gut barrier. This leaves the system vulnerable to future breaches and continued immune activation. The true advantage, as Bulsiewicz implies, lies in understanding this systemic dynamic. By nurturing the gut microbiome and strengthening the gut barrier, we address the root cause of chronic inflammation, shifting from a state of constant internal conflict to one of resilience and ease. This requires patience and a commitment to practices that support gut health, recognizing that the payoffs are not immediate but build over time, creating a durable foundation for well-being.
The Downstream Cost of Ignoring the Gut
The cascade effect of a compromised gut barrier extends beyond inflammation to impact energy levels and overall resilience. When the immune system is constantly activated, it expends significant energy fighting internal battles. This diverts resources that would otherwise be available for daily functioning, leading to fatigue and a sense of being in a perpetual state of "fight or flight."
The analogy of war is potent here: much like a physical war causes destruction to the surrounding environment, chronic immune activation can lead to self-inflicted bodily injury. This isn't a failure of the immune system, but rather a consequence of it being perpetually deployed due to breaches it shouldn't have to contend with. The immediate "solution" of immune activation, when the underlying cause (a leaky gut) is not addressed, becomes the source of long-term problems.
This highlights a critical failure of conventional wisdom, which often focuses on immediate symptom relief. While a temporary reduction in inflammation might feel productive in the moment, it fails to address the systemic breakdown. The real competitive advantage, in health terms, comes from understanding and acting upon these downstream consequences. Investing in gut health--through diet, lifestyle, and mindful choices--is an investment in long-term resilience, energy, and a robust immune system that is not constantly at war with itself. This requires a shift in perspective, recognizing that immediate discomfort or effort in healing the gut can lead to significant, lasting payoffs in overall vitality and health, creating a moat against the pervasive issue of chronic inflammation.
Key Action Items
- Immediate Action (Within the next week):
- Begin tracking food intake and noting any immediate digestive discomfort or energy fluctuations. This starts the process of understanding your personal gut-story.
- Incorporate one new gut-supportive food daily (e.g., fermented foods like kimchi or sauerkraut, high-fiber vegetables, or prebiotic-rich foods like onions and garlic).
- Short-Term Investment (Over the next quarter):
- Prioritize sleep hygiene: Aim for 7-9 hours of quality sleep per night, establishing a consistent bedtime and wake-up routine. This directly supports gut barrier function and immune regulation.
- Reduce intake of highly processed foods, refined sugars, and artificial sweeteners, which are known to negatively impact the gut microbiome.
- Introduce a daily mindfulness or stress-reduction practice (e.g., meditation, deep breathing exercises) for 10-15 minutes. This helps to shift the nervous system out of "fight or flight" and supports immune balance.
- Longer-Term Investment (6-18 months and beyond):
- Explore a diverse, whole-foods-based diet rich in fiber and resistant starches. This requires consistent effort but builds a robust and resilient gut microbiome, paying off in sustained energy and reduced inflammation.
- Consider consulting with a healthcare professional specializing in gut health or immunology to gain personalized insights and strategies for addressing chronic inflammation and improving gut barrier function. This investment in expert guidance can accelerate progress and prevent missteps.