The healthcare industry, long mired in technological inertia, stands on the precipice of a dramatic transformation driven by artificial intelligence. While medical advancements have soared, their delivery has lagged, creating a "technology slop" that burdens both patients and practitioners. This conversation with Dr. Robert Wachter and Dr. Pierre Elias reveals that AI is not merely an incremental improvement but the catalyst for a "giant leap," poised to address decades of systemic inefficiencies. The hidden consequences of this AI integration extend beyond mere efficiency, promising to democratize care and redefine the physician's role. Those who understand and strategically adopt these AI tools will gain a significant advantage in navigating the complex, evolving landscape of modern medicine.
The Slow Burn to a Sudden Revolution: Why AI is Healthcare's "Suddenly" Moment
For decades, the promise of artificial intelligence in healthcare felt like a distant, perpetually deferred revolution. Early attempts in the 1970s and 80s, focused on complex diagnostic problems with rudimentary "if-then" logic and paper-based data, predictably flamed out. IBM's Watson, after its Jeopardy triumph, stumbled in its healthcare ambitions, offering more sizzle than substance and proving too expensive and impractical for real-world clinical use. The subsequent digitization of medical records through Electronic Health Records (EHRs) was hailed as the gateway to innovation, akin to Amazon or Netflix, but instead, often created a "productivity paradox," making doctors data-entry clerks and increasing "pajama time" spent on administrative tasks.
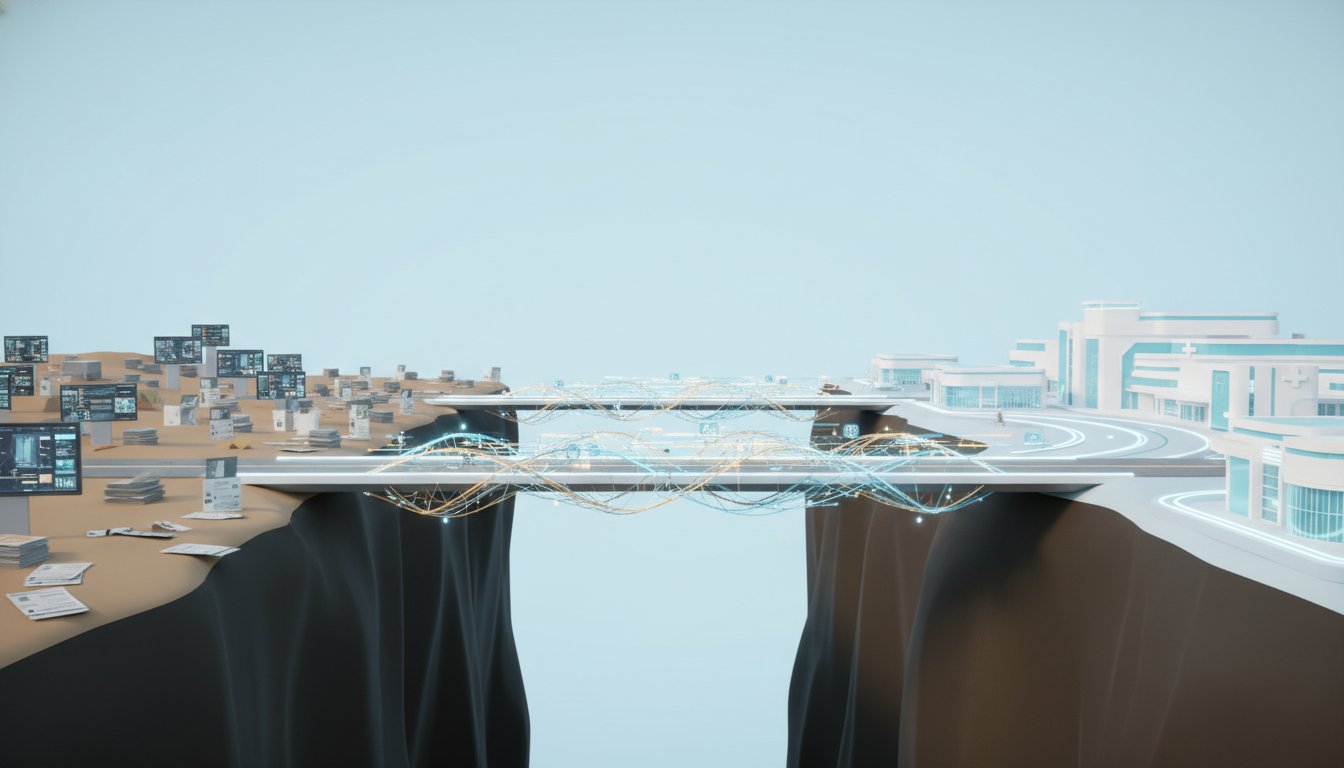
This era of gradual, often frustrating, progress has finally given way to a "suddenly" moment, as described by Robert Wachter, citing Hemingway. The convergence of advanced AI, particularly generative AI, with a healthcare system desperate for reform, is creating an unprecedented opportunity. The key difference now is a more strategic, eyes-open approach. Instead of tackling the hardest problems first, the focus has shifted to "low-hanging fruit"--AI tools that demonstrably improve workflows and reduce clinician burden without immediate, high-stakes risks. Digital scribes that auto-generate clinical notes and AI-powered chart summarization are prime examples. These tools don't threaten doctors' jobs; they aim to make them better at their jobs, alleviating the administrative overload that has plagued the profession.
"The giant leap really is the combination of the magic of the new AI meeting a healthcare system that's in desperate need of change, and everybody knows it. We really are about to have our suddenly moment when healthcare is actually transformed after tiptoeing our way toward this over the last 10 or 15 years to make it better and safer, more accessible, more satisfying for everybody, both patients and clinicians, and I think eventually less expensive, although that's a harder ask."
This shift from theoretical ambition to practical application is crucial. The failure of past initiatives wasn't solely a technological deficit; it was a failure to transform organizational structures, culture, and workflows alongside the technology. The current wave of AI adoption, by contrast, emphasizes integration and clinician partnership, recognizing that technology is only effective when it aligns with the human element of healthcare.
The Unseen Diagnostic Edge: AI's Ability to Find What Humans Miss
While digital scribes offer immediate relief, the true transformative power of AI in healthcare lies in its capacity for advanced diagnostics, uncovering conditions that elude even experienced clinicians. Pierre Elias, a cardiologist at Columbia University, highlights the limitations of current cardiovascular disease screening. Traditional methods like cardiac catheterization are too invasive for widespread use, and echocardiograms, while less invasive, are too expensive for population-level screening. This often means patients are diagnosed only after symptoms become severe, leading to worse outcomes.
AI, however, can leverage readily available, low-cost data sources, such as electrocardiograms (ECGs), to identify subtle patterns indicative of serious conditions. Elias's team developed an AI model, EchoNext, that can predict structural heart disease from an ECG with greater accuracy than a panel of cardiologists. This is not because the AI "thinks" like a doctor, but because it can detect correlations and patterns in vast datasets that are imperceptible to human observers.
"We did not; only the AI did. For a long time, we thought a holy grail would be if the AI could see something, tell us what it saw, and then we could teach it back to doctors. But it doesn't work that way. Modern AI techniques still don't do a very good job of explaining what the AI sees. The AI doesn't think the way a doctor does."
The implication here is profound: AI can act as a powerful diagnostic co-pilot, flagging high-risk patients who might otherwise fall through the cracks. The case of a young man with undiagnosed heart failure, identified by EchoNext and ultimately receiving a life-saving heart transplant, exemplifies this. This ability to proactively identify disease, especially in its early, asymptomatic stages, represents a significant leap towards preventative and more equitable healthcare. It offers a competitive advantage to healthcare systems that can integrate such predictive capabilities, leading to better patient outcomes and potentially lower long-term costs.
The "Wicked Problem" of Integration: Navigating Inertia, Incentives, and the Future of the Physician
The successful integration of AI into healthcare is not merely a technical challenge; it's a "wicked problem" fraught with historical baggage, competing incentives, and deeply ingrained human behaviors. Bob Wachter identifies a complex web of factors--history, politics, economics, pride, regulations, leadership, lawsuits, guilds, culture, workflows, inertia, greed, hubris, vibes, and zeitgeist--that will shape AI's impact, often more so than the technology itself.
The dominance of Electronic Health Record (EHR) giant Epic exemplifies this. While Epic's integrated system has been successful, its closed nature poses a significant barrier to third-party AI innovators. The company's "own the entire thing" philosophy, while beneficial for internal integration, can stifle external innovation and limit the adoption of best-in-class AI tools. The government's push for greater openness is a critical step, but overcoming the inertia of established players and the inherent complexity of healthcare workflows remains a substantial hurdle.
Furthermore, the specter of "deskilling" looms. While AI can augment physician capabilities, an over-reliance on AI decision support could, in theory, lead to a decline in fundamental clinical skills. The study of gastroenterologists whose performance dipped after a temporary AI tool was removed serves as a cautionary tale. The challenge, therefore, is to leverage AI to enhance, not erode, physician expertise.
"But although you do write about the fact that AIs can do better in the empathy realm than humans. That was one of the shockers, that in those early years, which is really only two years ago, when we saw AI passing the medical licensing board or doing well on really tough clinical cases, it was like, 'Okay, it's pretty smart.' And then studies began to come out saying, 'If you did a blinded trial of a patient actor being given answers either by doctors or by AI, they often preferred the answers from AI, and the AI appeared to be more empathic.'"
Ultimately, the physician's role is likely to evolve, not disappear. As AI handles more of the data analysis and diagnostic support, doctors will be freed to focus on the inherently human aspects of care: empathy, complex ethical decision-making, patient preference interpretation, and communication of difficult news. This shift requires a recalibration of medical education and a conscious effort to ensure that AI serves as a co-pilot, not a replacement, guiding physicians to be more effective and compassionate caregivers. The optimism for AI in healthcare, Wachter suggests, stems from the public's positive perception of its potential, recognizing the desperate need for reform in a system where simply hiring more humans is no longer a viable or affordable solution.
- Immediate Action: Adopt AI-powered digital scribes to reduce physician administrative burden and "pajama time." This offers immediate relief and improves clinician satisfaction.
- Short-Term Investment (0-6 months): Pilot AI diagnostic support tools for specific conditions (e.g., cardiovascular disease from ECGs) in controlled environments. Focus on tools that augment, rather than replace, existing clinical decision-making.
- Medium-Term Investment (6-18 months): Integrate AI-driven chart summarization tools into EHR systems to provide clinicians with rapid access to critical patient information, improving preparedness and reducing missed diagnoses.
- Strategic Focus (1-2 years): Develop internal expertise and partnerships to validate and deploy AI tools, ensuring they align with clinical workflows and patient needs. Prioritize AI applications that address known system inefficiencies or diagnostic gaps.
- Long-Term Investment (2-3 years): Advocate for greater interoperability and openness within EHR systems to facilitate the integration of third-party AI solutions, preventing vendor lock-in and fostering innovation.
- Cultural Shift (Ongoing): Reframe medical education to emphasize AI literacy and the evolving role of the physician as a strategic interpreter of AI-generated insights, focusing on empathy, complex decision-making, and patient advocacy.
- Discomfort for Advantage (Ongoing): Embrace the initial discomfort of adopting new AI workflows and the potential for AI to challenge established diagnostic practices, recognizing that this willingness to adapt is crucial for long-term competitive advantage and improved patient care.