Reversing Type 2 Diabetes Through Low-Carb Diet and Lifestyle Changes
TL;DR
- Reducing starchy carbohydrates dramatically improves blood sugar control, preventing the progression of insulin resistance and potentially reversing Type 2 diabetes.
- Poor metabolic health, indicated by fatigue, belly fat, and brain fog, is a root cause of serious conditions like cardiovascular disease and Alzheimer's.
- Low-carb diets can lead to significant weight loss and improved metabolic markers, often proving more effective than medication for Type 2 diabetes.
- Food addiction, particularly to ultra-processed carbohydrates, is a significant driver of chronic disease and requires targeted intervention for long-term health.
- It is never too late to improve metabolic health; lifestyle changes can reverse damage and enhance mood, energy, and cognition at any age.
- Many common chronic conditions, including joint pain and IBS, can improve by addressing diet, demonstrating the interconnectedness of metabolic health.
- Healthcare professionals must provide informed consent by explaining the pros and cons of medications and lifestyle changes to empower patient choices.
Deep Dive
Dr. David Unwin, an NHS GP, presents a compelling case that type 2 diabetes and associated metabolic dysregulation are not inevitable chronic conditions but are largely reversible through dietary and lifestyle changes. His personal journey and extensive patient data demonstrate that a significant portion of individuals with type 2 diabetes can achieve drug-free remission by adopting a low-carbohydrate, whole-foods approach. This insight challenges the prevailing medical paradigm of lifelong medication and suggests a more empowering, patient-centered model of care focused on addressing the root causes of metabolic disease.
The primary driver of these metabolic issues, according to Unwin, is insulin resistance, often exacerbated by excessive consumption of starchy carbohydrates and ultra-processed foods. These foods break down into sugar, leading to elevated blood glucose and, consequently, increased insulin production. Over time, this constant demand on the pancreas, coupled with the accumulation of fat in the liver and pancreas, impairs insulin's effectiveness. Unwin highlights that symptoms like fatigue after meals, increased belly fat, and cognitive fog are early indicators of this decline, often misattributed to normal aging. His own experience, marked by these symptoms and a type 2 diabetes diagnosis, dramatically reversed through a low-carb diet, underscores the potential for profound personal transformation.
This approach has significant second-order implications for healthcare systems and individual well-being. By demonstrating tangible results--including drug-free remission rates of 50% in his practice and substantial cost savings on diabetes medication--Unwin provides evidence that lifestyle interventions can be as, if not more, effective than conventional treatments. This challenges the traditional paternalistic medical model, advocating for informed consent where patients are presented with lifestyle change as a viable alternative to lifelong medication. Furthermore, the widespread normalization of poor metabolic health, including the alarming rise in type 2 diabetes in young people, suggests a societal shift that demands proactive, preventative strategies. Unwin's data indicates that earlier intervention, particularly for pre-diabetes, yields higher remission rates, emphasizing the critical importance of addressing metabolic health before chronic conditions fully manifest.
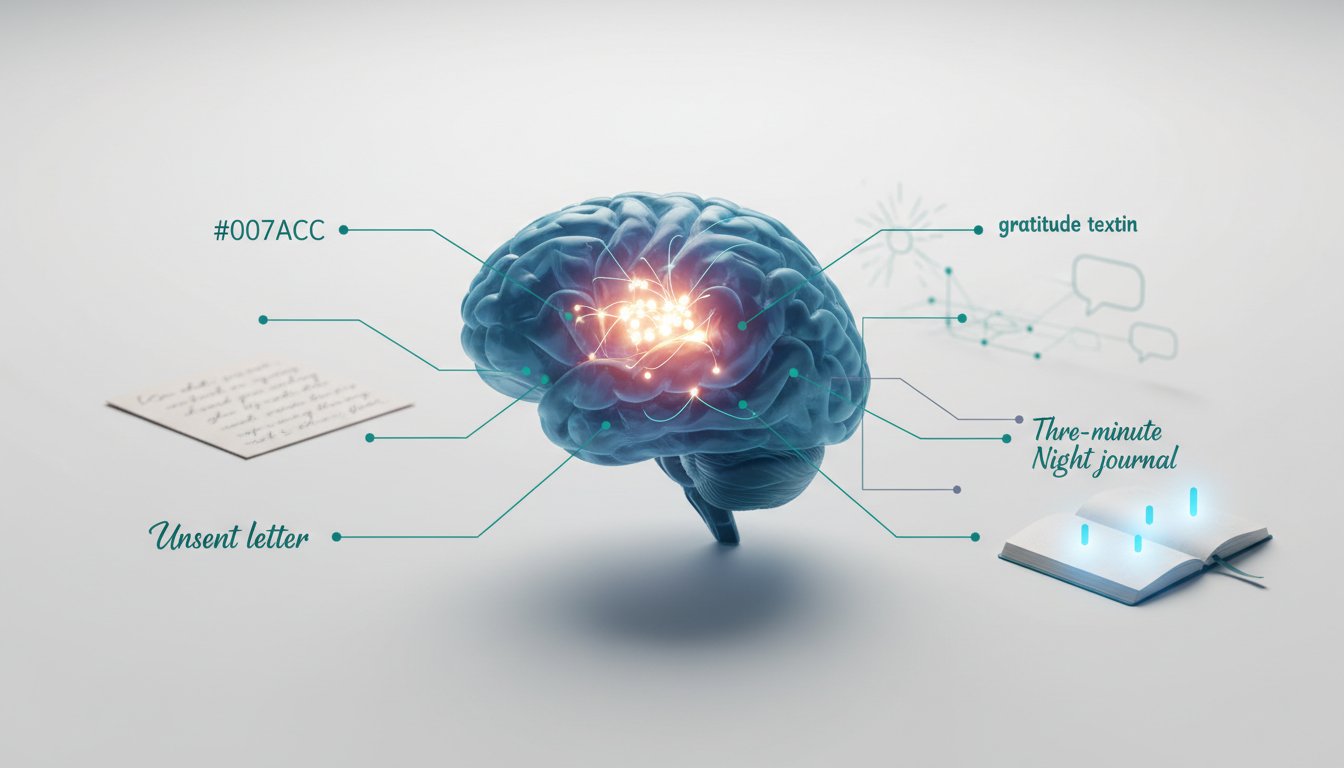
The implications extend beyond diabetes management. Unwin notes that patients adopting a low-carb, whole-foods diet often experience improvements in a wide range of conditions, including joint pain, eczema, psoriasis, irritable bowel syndrome, sleep apnea, and even mood disorders. This suggests a systemic impact of diet on overall health, where addressing the root of metabolic dysfunction can unlock widespread improvements. The concept of food addiction, particularly to ultra-processed foods, is also presented as a critical barrier to sustained health. Unwin argues that recognizing and addressing addictive behaviors around food is essential for long-term remission, as temporary dietary changes may not be sufficient if the underlying addiction remains unaddressed. His wife, a clinical health psychologist, has pioneered research in this area, demonstrating clinical outcomes for food addiction treatment.
Ultimately, the core message is that metabolic health is not fixed and can be significantly improved, offering a pathway to not only reversing type 2 diabetes but also enhancing overall vitality and well-being. Unwin's work advocates for a paradigm shift towards empowering individuals with knowledge and choices, fostering a more preventative and patient-centered approach to healthcare that prioritizes addressing the fundamental drivers of chronic disease.
Action Items
- Audit metabolic health: For 5-10 patients, measure fasting insulin and triglycerides to identify early insulin resistance.
- Create patient education materials: Develop 3-5 visual aids explaining the "teaspoons of sugar" equivalent for common carbohydrate-rich foods.
- Design a "food addiction" screening tool: Adapt existing criteria to identify individuals struggling with ultra-processed food consumption within a patient population.
- Implement a 30-minute consultation protocol: For patients initiating lifelong medication, dedicate 30 minutes to discuss pros, cons, and collaborative decision-making.
- Track patient outcomes on low-carb diets: For 50-100 patients, monitor HbA1c, blood pressure, and lipid profiles at 3-year intervals to validate effectiveness.
Key Quotes
"only one in eight of the population is metabolically healthy one in eight so in our practice of all the people who have diabetes we know that if they go low carb 50 of them will achieve drug free type two diabetes remission at three years further 48 have improved their blood sugar significantly or maybe they're on less medication it's amazing because the average improvements are better than drugs for diabetes"
Dr. Rangan Chatterjee introduces Dr. David Unwin's practice data, highlighting the significant success rate of patients achieving drug-free type 2 diabetes remission or improved blood sugar control through a low-carb approach. This statistic suggests that lifestyle interventions can be more effective than conventional medication for managing diabetes.
"And this is a serious issue because poor metabolic health is one of the root cause drivers of insulin resistance, type two diabetes, cardiovascular disease, strokes, Alzheimer’s and many forms of cancer."
Dr. Chatterjee emphasizes the widespread impact of poor metabolic health, identifying it as a foundational cause for a range of serious chronic diseases. This underscores the importance of addressing metabolic health proactively to prevent a cascade of health problems.
"The first thing is I used to find myself tired particularly after meals so I remember after lunch even in the practice I'd have to have a little nap on my own doctor's couch isn't that terrible and I was only 55 I and I thought that was aging so the first thing is tiredness particularly after meals and also I was always ready to lie down in the evening I was always thinking I'd put my feet up instead of doing anything that's one thing"
Dr. David Unwin shares his personal experience with early signs of poor metabolic health, describing post-meal fatigue and evening lethargy as symptoms he initially attributed to normal aging. This personal anecdote illustrates how common symptoms can be overlooked as indicators of underlying metabolic issues.
"And my insulin wasn't working properly I mean and then you have the various biochemical tests that doctors might do so uh any sign of fatty liver well maybe we'll come on to that a third of everybody in the world now has fatty liver so I had that as well"
Dr. Unwin connects his personal symptoms to the physiological issue of insulin resistance and mentions fatty liver as another common biochemical marker associated with poor metabolic health. He highlights that conditions like fatty liver are widespread, suggesting a systemic problem with metabolic regulation.
"And my insulin wasn't working properly I mean and then you have the various biochemical tests that doctors might do so uh any sign of fatty liver well maybe we'll come on to that a third of everybody in the world now has fatty liver so I had that as well"
Dr. Unwin connects his personal symptoms to the physiological issue of insulin resistance and mentions fatty liver as another common biochemical marker associated with poor metabolic health. He highlights that conditions like fatty liver are widespread, suggesting a systemic problem with metabolic regulation.
"And I believe there's something very peculiar about that I'm it's interesting because I i lecture at edge hill university sometimes I'm an honorary lecture in medical ethics and it is so odd that we're doing things to patients without explaining the pros and cons and how is it that we're exempt from giving people that vital information for for like say metformin I know that approximately a third of people given metformin over 10 years will find them get diarrhea like that lady and yet I didn't have to tell her it's odd isn't it why do you think that is so peculiar"
Dr. Chatterjee expresses concern about the lack of informed consent regarding lifelong medications like metformin, noting that patients are often not fully informed about potential side effects. He finds this practice peculiar, especially in contrast to the detailed consent required for minor procedures.
"So I remember a time when I was little when most people were were fit I didn't know anybody with type two diabetes or asthma I didn't know any children or young people with depression the world was so different and I I think we're beginning to normalize chronic ill health and the danger of that"
Dr. Unwin reflects on a past era where chronic illnesses like type 2 diabetes and depression were less prevalent among the general population. He expresses concern that society is becoming desensitized to these conditions, normalizing what was once considered abnormal.
"So I remember a time when I was little when most people were were fit I didn't know anybody with type two diabetes or asthma I didn't know any children or young people with depression the world was so different and I I think we're beginning to normalize chronic ill health and the danger of that"
Dr. Unwin reflects on a past era where chronic illnesses like type 2 diabetes and depression were less prevalent among the general population. He expresses concern that society is becoming desensitized to these conditions, normalizing what was once considered abnormal.
"So I remember a time when I was little when most people were were fit I didn't know anybody with type two diabetes or asthma I didn't know any children or young people with depression the world was so different and I I think we're beginning to normalize chronic ill health and the danger of that"
Dr. Unwin reflects on a past era where chronic illnesses like type 2 diabetes and depression were less prevalent among the general population. He expresses concern that society is becoming desensitized to these conditions, normalizing what was once considered abnormal.
"So I remember a time when I was little when most people were were fit I didn't know anybody with type two diabetes or asthma I didn't know any children or young people with depression the world was so different and I I think we're beginning to normalize chronic ill health and the danger of that"
Dr. Unwin reflects on a past era where chronic illnesses like type 2 diabetes and depression were less prevalent among the general population. He expresses concern that society is becoming desensitized to these conditions, normalizing what was once considered abnormal.
"So I remember a time when I was little when most people were were fit I didn't know anybody with type two diabetes or asthma I didn't know any children or young people with depression the world was so different and I I think we're beginning to normalize chronic ill health and the danger of that"
Dr. Unwin reflects on a past era where chronic illnesses like type 2 diabetes and depression were less prevalent among the general population. He expresses concern that society is becoming desensitized to these conditions, normalizing what was once considered abnormal.
"So I remember a time when I was little when most people were were fit I didn't know anybody with type two diabetes or asthma I didn't know any children or young people with depression the world was so different and I I think we're beginning to normalize chronic ill health and the danger of that"
Dr. Unwin reflects on a past era where chronic illnesses like type 2 diabetes and depression were less prevalent among the general population. He expresses concern that society is becoming desensitized to these conditions, normalizing what was once considered abnormal.
"So I remember a time when I was little when most people were
Resources
External Resources
Books
- "Beat the Diet Trap" by Dr. Berrifer - Referenced as the book that helped Dr. Unwin's wife rethink food and insulin resistance.
Articles & Papers
- BMJ Nutrition 2023 paper - Discussed as the source for data showing improved cardiovascular risk markers in Dr. Unwin's patients.
- Paper on glycemic load by Dr. Jeffrey Lustig and Dr. Unwin - Published to provide teaspoon of sugar equivalents for commonly eaten foods.
- Swedish paper on ultra-processed food addiction - Cited as evidence that ultra-processed food addicts are 600% more likely to develop type two diabetes.
- Paper on liver fat accumulation by Professor Roy Taylor - Explained as central to reversing type two diabetes.
People
- Dr. David Unwin - Guest GP who reversed his own type two diabetes and helped over 150 patients do the same.
- Dr. Rangan Chatterjee - Host of the podcast "Feel Better, Live More."
- Dr. Jeffrey Lustig - Expert on glycemic load, co-authored a paper with Dr. Unwin.
- Professor Roy Taylor - Friend of Dr. Unwin, senior author on his paper, known for work on type two diabetes and low-calorie diets.
- Dr. Mickey Ben Dov - Worldwide expert on what cavemen ate, discussed ancestral diets.
- Professor Wong - Local professor of nephrology, collaborated with Dr. Unwin to study kidney function in diabetic patients.
- Christine Delon - Medical statistician who assisted Dr. Unwin with analyzing his practice data.
- Henry Shukman - Creator of the "The Way" meditation app, former guest on the podcast.
Organizations & Institutions
- NHS (National Health Service) - The UK's public healthcare system where Dr. Unwin practices.
- Public Health Collaboration - A UK charity co-founded by Dr. Unwin and Dr. Chatterjee, offering free resources on diet and health.
- The Way App - A meditation app offering a unique, choice-free approach to establishing a practice.
- Do Health - A personalized health companion app co-founded by Dr. Chatterjee.
- The Caldesi - Low-carb chefs with whom Dr. Unwin has co-authored recipe books.
Websites & Online Resources
- Freshwell App - A free app providing low-carb recipes on a budget, approved by the NHS.
- X (formerly Twitter) - Platform where Dr. Unwin (low carb gp) shares information and interacts with a global community.
- D Life India - A website offering vegan and vegetarian recipes, particularly for Asian diets, and assisting with type two diabetes remission.
Other Resources
- Continuous Glucose Monitor (CGM) - A device used to track blood sugar levels, discussed as a tool for patient education.
- Metformin - A baseline medication for type two diabetes, discussed in relation to side effects and patient experience.
- Keto diet - A type of low-carb diet focused on burning fat.
- Ketosis - A metabolic state where the body burns fat for fuel.
- Ketoacidosis - A serious condition, distinguished from ketosis, often seen in type one diabetes.
- Ultra-processed food addiction - A concept discussed as a significant factor in chronic disease and difficulty with dietary changes.
- Industrial seed oils - Discussed as potentially inflammatory and advised against by Dr. Unwin.
- Teaspoon of sugar infographics - Visual aids developed by Dr. Unwin and colleagues to illustrate the sugar content of foods.
- NICE guidelines - National Institute for Health and Care Excellence guidelines, discussed in the context of medical practice and adherence.